How can we Reduce Indwelling Urinary Catheter Use and Complications?
Case
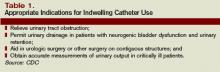
A 68-year-old male with a history of Alzheimer’s dementia and incontinence presents with failure to thrive. A Foley catheter is placed due to the patient’s incontinence and fall risk. Three days after admission while awaiting placement in a skilled nursing facility (SNF), he develops a urinary tract infection (UTI) complicated by delirium delaying his transfer to the SNF. What could have been done to prevent this complication?
Overview
It has been 50 years since Beeson, et al., recognized the potential harms stemming from urethral catheterization and penned an editorial to the American Journal of Medicine titled “The case against the catheter.”1
Since then, there has been considerable exploration of ways to limit urethral catheterization and ultimately decrease catheter-associated urinary tract infections (CAUTIs). Unfortunately, little progress has been made; indwelling urinary catheters remain ubiquitous in hospitals and CAUTIs remain the most common hospital-acquired infection in the United States.2 Given the emphasis on the quality and costs of healthcare, it is an opportune time to revisit catheter management and use as a way to combat the clinical and economic consequences of CAUTIs.
Clinicians may be lulled into thinking the clinical impact of CAUTI is less than that of other nosocomial infections. However, beyond the obvious patient harm from UTIs, associated bacteremia, and even death, the public health implications of CAUTI cannot be denied. Urinary tract infections constitute 40% of all nosocomial infections; accounting for an estimated 1 million cases annually.3 Further, 80% of all UTIs are associated with indwelling catheter use.
On average, nosocomial UTI necessitates one extra hospital day per patient, or approximately one million excess hospital days per year.4 Pooled cost analysis shows that UTIs consume an additional $400-$1,700 per event, or an estimated $425 million per year in the United States.5,6 Clearly, we cannot wait another 50 years to address this problem.
Review of the Data
Catheter duration as a risk factor for CAUTI: The indwelling catheter creates a portal of entry into a usually sterile body cavity and provides a surface on which microorganisms can colonize. At a finite rate of colonization—the incidence of bacteriuria is 3% to 10% per catheter day—the duration of urinary catheterization becomes the strongest predictor of catheter-associated bacteriuria.7 Even in relatively short-term catheter use of two to 10 days, the pooled cumulative incidence of developing bacteriuria is 26%.
Given the magnitude of these numbers, it should be no surprise that after one month of catheterization, bacteriuria develops in almost all patients. Twenty-four percent of patients with bacteriuria develop symptomatic UTIs with close to 5% suffering bacteremia. Consequently, nosocomial UTIs cause 15% of all hospital-acquired bacteremia.