The Dutch Medical Education
Editors’ note: During 2006 we will publish coverage of hospital practices in other countries. This is the second article in that effort. Our first article, on the state of hospital medicine in Afghanistan, was published in the Jan. issue on p. 1.
For the first time in the Netherlands, the Free University of Amsterdam has appointed three professors in two non-university hospitals with a specific assignment for teaching. Until now, professors in such hospitals were appointed only for a specific research task that they perform in—or in close collaboration with—the university. In this article we describe the reasons and expectations for these appointments.
Medical Training in the Netherlands
Both undergraduate and postgraduate training in the Netherlands takes place in eight university medical centers. Although preclinical teaching is mainly a university domain, around two-thirds of the clinical training for interns and residents takes place in “affiliated” non-university teaching hospitals.
Until recently, medical education consisted of four years of preclinical studies and two years of clinical training. Now students are gradually admitted into the clinic during their first or second year of medical education. Further, the Dutch government has ruled that the number of first-year medical students must increase by 40. Both measures will result in a significant increase in the number of interns in the coming years.
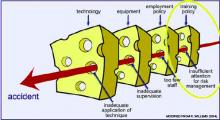
Because university hospitals presently accommodate the maximum number of interns they can take, the participation of non-university hospitals will rise considerably. However, their role must take into consideration not only quantity, but also quality. Because more than 90% of care in the Netherlands is delivered in non-university hospitals, these institutions provide the most proper setting for contextual learning. Adequate training is a prime barrier against accidents, so more resources must be invested in the quality of training programs in non-university hospitals to ensure the quality of future health care in the Netherlands.1,2 (See “Barriers Against Accidents,” p. 41.)
Teaching in Non-University Hospitals
By definition, medical education should be a core objective for teaching hospitals. (See “Requirements for Teaching Hospitals,” at right) This requires wide involvement by hospitals. Doctors in university hospitals generally have a contractual obligation to participate in teaching as part of their appointment. For most doctors in non-university hospitals, teaching is not part of their contract. Yet many of them do so on a voluntary basis. The advantage is that they are intrinsically motivated; however, the consequence is that they are not professional teachers, but rather well-meaning amateurs. This problem was recently addressed by the Central College for Medical Specialists, the ruling committee for specialist training in the Netherlands. Program directors and other specialists involved in teaching now take special courses to develop their teaching abilities.
Another issue involves defining end goals and planning curricula.3 For interns the goals are outlined in the “Blueprint for the Training of Medical Doctors in the Netherlands”; however, in practice, most internships are not structured, and learning opportunities depend on patient availability.4 It’s even questionable to what extent the precise curricular goals are known to interns and doctors alike.
For specialists, the end goals used to be inferred from practice, leaving lots of room for individual interpretation in the local institutions. These end goals are only now being defined. Many practical dilemmas, such as the relative weight we award to the various competencies, remain. For example, how much time should a surgical resident spend inside and outside the operating room? And what is the relative importance of experience? A key problem is that instruments that reliably measure the acquired competencies and the efficiency and efficacy of clinical training programs are still in their infancy.