Over the past two decades, quality improvement and patient safety (QI/PS) have become integral to the mission of hospital medicine, driving system-wide problem solving and practice changes to improve patient care. With the introduction of the Accreditation Council for Graduate Medical Education requirements to integrate QI/PS activities into graduate medical education, the significance of structured QI/PS work and its incorporation into promotion criteria, especially for academic hospitalists, has become increasingly evident.1
Additionally, early-career academic hospitalists identify meaningful engagement in QI/PS projects as critical factors for their professional satisfaction and development.2 The role of QI/PS activities in the growth and promotion of academic hospitalists was also underscored in a recent scoping review on faculty development in academic hospital medicine.3 Therefore, integrating QI/ PS activities into the four pillars of hospital career satisfaction identified by the Society of Hospital Medicine not only supports the professional development of hospitalists but also aligns their work with institutional missions and patient care improvement.4
However, other than peer-reviewed publications, identifying promotional scholarship in QI/PS has been challenging in traditional academic pathways.5 We set out to systematically capture QI/PS activities and promote their recognition at our institution.
Solution Overview
Our efforts culminated in the Practitioner Leads in Quality & Safety Merit Pathway, or PLQS Award for simplicity, within our medicine service line, which includes the hospital medicine section. The goals of this program were to 1) catalog QI/PS activities conducted by hospital medicine practitioners and other clinicians, ensuring that all initiatives comply with approved guidelines and do not involve unapproved research, 2) establish award mechanisms to recognize those efforts, thereby enhancing recipients’ curricula vitae, 3) coach the development and execution of QI/ PS projects using robust methodology, and 4) support the generation of scholarly work. Prior to this, QI/ PS activities across the medicine service were largely ad hoc, pursued in isolated pockets with varying degrees of support and poor visibility, unless they achieved publication.
Implementation Process
Implementation of the PLQS Award was first chartered and then approved as a non-research QI project sponsored by the chief of the medicine service line. A set of outcome, process, and structure measures was compiled, which included:
- Number of PLQS Award recipients each year (outcome measure)
- Operational impact, both locally and beyond, is categorized as yes or no (outcome measure)
- Scholarship evidenced by conference presentations or publications, categorized as yes or no for each (outcome measure)
- Project progression and final disposition (hybrid outcome and process measure)
- Clinical section affiliation (structure measure)
- Presence of multidisciplinary project team, categorized as yes or no (structure measure)
- Involvement of medical trainees, categorized as yes or no (structure measure)
All measures were tracked in a Microsoft Excel spreadsheet by one of the authors (CW), a hospital medicine provider with 50% full-time equivalent allocation to manage our institution’s QI office. This office, alongside the medical center’s Human Research Protection Program, shares responsibility for classifying projects as either research or non-research. Through this review process, which acted as a natural funnel for cataloging QI/ PS activities, PLQS Award candidates were conveniently identified. In return, PLQS procedures encouraged compliance with hospital policies, as only projects officially approved as non-research could qualify for the award.
Projects classified as non-research were subsequently inducted into the PLQS Award database. Project progress was monitored, and core measures were updated every six months through brief check-ins with team members until one of three outcomes materialized: 1) the adoption of changes into everyday workflow, 2) conclusion without adoption or completion of analysis if no intervention was performed, or 3) cancellation. Demonstrable effort, identified through these regular reviews, was honored with the PLQS Award for one year.
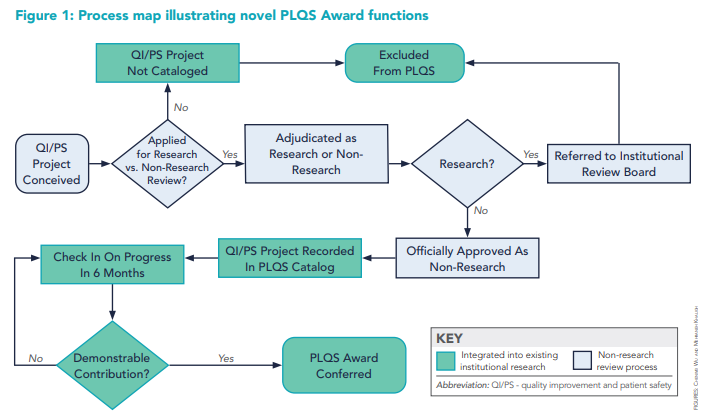
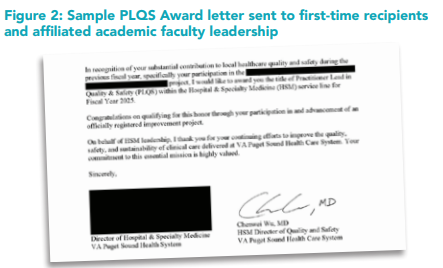
Figure 1 illustrates the integration of the novel PLQS Award functions into the existing research versus non-research review process. The award was automatically renewed if QI/PS contributions were sustained beyond the first year. Newly inducted and renewing PLQS Award recipients’ names were announced at a medicine staff meeting, and letters of recognition were sent to first-time honorees and affiliated academic leadership. (Figure 2) A notice about the award also appeared in the departmental electronic newsletter.
Our historical experience over the past five years indicates that a commitment of approximately six hours per year was sufficient to sustain PLQS Award functions, including database maintenance, preparation of letters of recognition using a standard template, and award presentations. This commitment was in addition to an initial six-hour investment required to program the master spreadsheet and design the template for the letters of recognition. Reflecting on this time allotment, we found that managing the PLQS Award imposed only a minor burden and was well-suited for a hospitalist with dedicated QI/PS time to oversee.
Outcomes and Impact
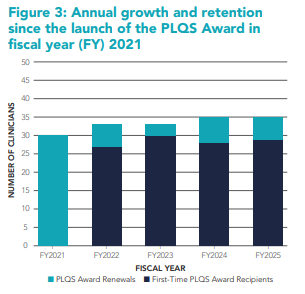
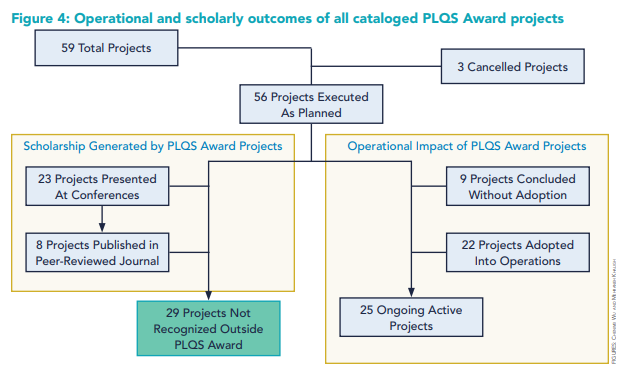
Since the implementation of our PLQS Award in 2021, between 30 and 35 clinicians annually have been recognized for their demonstrable contributions to approved QI/PS projects. In each of the past five years, three to eight PLQS Award recipients (average, 16% of the annual roster, ranging from 9% to 20%) were new inductees, while the majority consisted of renewals from the preceding year. (Figure 3) PLQS Award recognition has been conferred to 52 unique individuals across the program’s lifespan, of whom 19 (37%), including both authors, have earned the award in four or more consecutive years. Over the same period, 59 projects were cataloged, with 56 (95%) progressing to full-fledged analysis or implementation. Of these 56 projects, 27 (48%) led to scholarship traditionally valued in academic promotion, specifically 23 (41%) resulting in conference presentations and eight (14%) in publications. Importantly, the remaining 29 projects (52%) without scholarship would not have earned recognition outside of the PLQS Award. Figure 4 shows the operational and scholarly outcomes of all cataloged PLQS Award projects. Some published projects were never presented at conferences. Hence, the counts for presentations and publications are neither independent nor fully overlapping.
Operationally, 33 out of 56 non-canceled projects (59%) resulted in local practice changes, while four (7%) yielded regional or national impact. (Figure 4) Thirty-eight projects (68%) were multidisciplinary, and 23 (41%) incorporated medical trainees. The PLQS Award has been cited by name in faculty promotion highlights, including for individuals advancing to full professor rank. The reception from both PLQS Award recipients and academic leadership has been resoundingly positive, as highlighted in the following representative quotes:
- “Well, this is a nice little surprise. Thanks for all your help with this project. I didn’t know what I was doing when I started.”
- “[Dr. A] is fabulous. It’s nice to see her recognized for her QI and patient safety work. Thanks for the note, and we’ll get this in our division records.”
- “This is such exciting news! Congratulations to [Dr. B]! I will share this with the division.”
- “[Dr. C] has been a wonderful chief resident this year, and I’m so happy to see her get this recognition.”
Lastly, the PLQS Award has provided significant value to hospital leadership by safeguarding research funding through careful review of both research and non-research projects. Additionally, it has supported the Joint Commission Hospital Accreditation process by including the project catalog in survey materials, and it has strengthened Accreditation Council for Graduate Medical Education accreditation by reporting medical trainee participation to our affiliated graduate medical education office.
Lessons Learned
The PLQS Award represents a small-footprint, low-effort intervention with the potential to deliver significant value to hospital medicine providers engaged in QI/PS activities, especially at academic centers where promotion traditionally hinges on research and publication. Incorporating the PLQS Award model into established incentive structures, such as pay-for-performance, is similarly attractive. By customizing tracked measures, it can also be adapted to benefit a wider range of operational and educational stakeholders, as we have done. We believe the key to successfully replicating our model elsewhere lies in effectively integrating it into established research versus non-research review procedures at those sites. Without such a framework, the workload required to routinely and systematically identify qualifying QI/PS activities may become prohibitively high.
Future Directions
Although project coaching services were offered in the initial implementation phase of the PLQS Award, few individuals used them. Instead, many have used it as a central hub to inquire about research versus non-research criteria and clarify other technicalities. While we fully intend to retain this consultative function, we hope to intensify efforts around the third and fourth pieces of our objectives: coaching QI/PS projects from execution to scholarly translation. This might involve introducing more advanced QI concepts, such as run charts and statistical process control charts, encouraging the use of the Standards for Quality Improvement Reporting Excellence (SQUIRE 2.0) writing guidelines, or recommending journals that frequently accept QI/PS manuscripts.6,7 If such elements can be fully developed and assembled, they could create a standard pathway for the regular and reliable production of QI/PS scholarship, further enhancing career advancement opportunities in academic hospital medicine.

Dr. Wu

Dr. Khalighi
Dr. Wu is an assistant professor in the division of general internal medicine at the University of Washington and a hospitalist physician and director of quality and safety for hospital and specialty medicine at the VA Puget Sound Health Care System in Seattle. Dr. Khalighi is a clinical associate professor of medicine at the University of Washington and director of the preoperative medicine consult clinic at the VA Puget Sound Health Care System in Seattle.
Key Points
- Quality improvement and patient safety play a central role and have become core to hospital medicine, improving patient care and driving systemic changes.
- Hospitalists view QI/PS activities as essential for professional satisfaction, yet identifying and promoting QI/PS scholarship remains difficult in traditional academic pathways.
- The PLQS Award model requires minimal time investment, operates efficiently with limited resources, and allows for tailored tracking of measures to meet diverse needs.
- The PLQS Award has enhanced workplace visibility, practice change, and scholarly output by systematically cataloging QI/ PS activities and offering recognition, coaching, and support for scholarly work.
References
1. Accreditation Council for Graduate Medical Education. CLER pathways to excellence. ACGME website. https://www.acgme.org/globalassets/PDFs/CLERBrochure.pdf. Published 2014. Accessed October 5, 2025.
2. Cumbler E, et al. What is career success for academic hospitalists? A qualitative analysis of early-career faculty perspectives. J Hosp Med. 2018;13(6):372-377. doi: 10.12788/jhm.2924.
3. Misky GJ, et al. Faculty development in academic hospital medicine: a scoping review. J Gen Intern Med. 2023;38(8):1955-1961. doi: 10.1007/s11606-023-08089-4.
4. McKean S, et al. A challenge for a new specialty: a white paper on hospitalist career satisfaction. Canadian Society of Hospital Medicine website. https://canadianhospitalist.ca/system/files/CareerSatisfactionWhitePaper.pdf. Published December 2012. Accessed October 5, 2025.
5. Staiger TO, et al. Recognizing quality improvement and patient safety activities in academic promotion in departments of medicine: innovative language in promotion criteria. Am J Med. 2016;129(5):540-6. doi: 10.1016/j. amjmed.2016.01.006.
6. Amin SG. Control charts 101: a guide to health care applications. Qual Manag Health Care. 2001;9(3):1-27. doi: 10.1097/00019514-200109030-00003.
7. Ogrinc G, et al. SQUIRE 2.0 (standards for quality improvement reporting excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf. 2016;25(12):986-992. doi: 10.1136/bmjqs-2015-004411.