What Are the Clinical Indications for Noninvasive Positive Pressure Ventilation?
Case
A 63-year-old man with severe chronic obstructive pulmonary disease (COPD) presents with one week of increasing sputum, cough, and dyspnea. His respiratory rate is 26/minute and oxygen saturation is 86% on room air (RA). He is lethargic and appears mildly uncomfortable, but he responds appropriately to questions in three- to four-word sentences. He is tachypneic with accessory muscle use and has diffuse wheezes throughout his bilateral lung fields. His initial room air arterial blood gas (ABG) is 7.32/68/86/32. Chest radiograph is notable for flattened hemidiaphragms without focal opacity. The patient is placed on oxygen and receives prednisone with nebulized albuterol and ipratropium, but his dyspnea and tachypnea persist. Due to his respiratory distress, bilevel positive airway pressure (BiPAP) is considered.
What are the clinical indications for noninvasive positive pressure ventilation (NPPV)?
Overview
NPPV assists ventilation by delivering positive expiratory and/or inspiratory pressure without the use of an endotracheal tube. Theoretically, NPPV is a preferred method of ventilation as it may eliminate the need for endotracheal intubation and its associated morbidity and mortality, including airway trauma, loss of airway defense mechanisms (ventilator-associated pneumonia), mechanical ventilation (barotrauma), and disruption of speech and swallowing.1
NPPV is generally delivered via full-face mask or nasal mask. Nasal mask is often preferred for patient comfort, though air leaks occur with mouth breathing. There is no difference between nasal and full-face masks in outcomes including intubation rates and mortality.2,3,4 NPPV can be delivered via a portable or standard ventilator using the same modes available for endotracheal intubation, though pressure-cycled ventilators utilizing continuous positive airway pressure (CPAP) and BiPAP are most common. CPAP delivers air at a continuous fixed pressure throughout the respiratory cycle. BiPAP delivers positive pressure at alternating levels—higher for inspiration and lower for expiration. Guidelines suggest choosing a mode based on the etiology and pathophysiology of the respiratory failure and leveraging local comfort and expertise.2,3
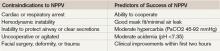
In general, good candidates for NPPV display signs of tachypnea and dyspnea due to hypoxic or hypercapnic respiratory failure but are hemodynamically stable, without excessive secretions, and can protect their airway and achieve a proper seal with the mask.3 Difficulty may arise due to patient intolerance, claustrophobia, gastric distention, and poor fit that leads to air leak or skin erosion. With initiation of NPPV, patients should be followed in a care setting with the capacity for frequent monitoring and, if needed, quick access to invasive airway management. Monitoring should include patient comfort and ability to tolerate the device, vital signs, breathing pattern, oxygen saturation, ABG, and mental status. This initial evaluation may help predict the success of NPPV (see Table 2). Appropriately chosen candidates who do well with NPPV often demonstrate respiratory turnaround in a relatively brief interval.2,3
Review of the Data
NPPV is increasingly utilized in a variety of clinical situations. In 2000, the American Thoracic Society published consensus guidelines on the use of NPPV in acute respiratory failure.2 More recently, the Canadian Medical Association developed clinical guidelines for the use of NPPV in the acute-care setting.4 Clinical scenarios in which there is evidence for the efficacy of NPPV include severe exacerbations of COPD, cardiogenic pulmonary edema, immunosuppressed patients with pulmonary infiltrates, and hypoxia; it can also be used as a bridge to extubation in COPD patients.1-4