Cut Costs, Improve Quality and Patient Experience
“Now that’s a fire!”
—Eddie Murphy
This is the final column in my five-part series tracing the history of the hospitalist movement and the factors that propelled it into becoming the fastest growing medical specialty in history and the mainstay of American medicine that it has become.
In the first column, “Tinder & Spark,” economic forces of the early 1990s pushed Baby Boomer physicians into creative ways of working in the hospital; a seminal article in the most famous journal in the world then sparked a revolution. In part two, “Fuel,” Generation X physicians aligned with the values of the HM movement and joined the field in record numbers. In part three, “Oxygen,” I explained how the patient safety and quality movement propelled hospitalist growth, through both inspiration and funding, to new heights throughout the late 90s and early 2000s. And in the October 2014 issue, I continued my journey through the first 20 years of hospital medicine as a field with the fourth installment, “Heat,” a focus on the rise in importance of patient experience and the Millennial generation’s arrival in our hospitalist workforce.
That brings us to the present and back to a factor that started our rise and is becoming more important than ever, both for us as a specialty and for our success as a country.
The Affordability Crisis
We have known for a long time how expensive healthcare is. If it wasn’t for managed care trying to control costs in the 80s and 90s, hospitalists might very well not even exist. But now, it isn’t just costly. It is unaffordable for the average family.
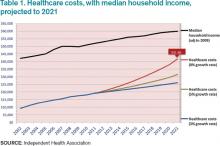
Table 1 shows projected healthcare costs and growth curves through 2021, with a median four-person household income overlaid.
In most scenarios, the two lines, income and healthcare costs, continue to get closer and closer—with healthcare costs almost $42,000 per family by 2021 in the most aggressive projection (8% growth). I am sure many of you have heard the phrase “bending the curve.” That simply means to try and bend that red line down to something approximating the blue line. It is slowing the growth, not actually decreasing the cost.
But it’s a step.
Only at that slowest healthcare growth rate projection (3%) does household income maintain pace. At the highest projection, two-thirds of family income will go toward healthcare. It simply won’t work. Affordability must be addressed.
Hospitalists are at the center of this storm. If you look at the various factors contributing to costs, we (and our keyboards) have great control and influence over inpatient, professional services, and pharmacy costs. To our credit, and to the credit of our teammates in the hospital, we actually seem to be bending the curve down toward the 5% range in inpatient care and professional services. Nevertheless, even at that level it is outpacing income growth.
In 2013, total healthcare costs for a family of four finally caught up with college costs. It is now just north of $22,000 per year for both healthcare costs and the annual cost of attending an in-state public college. Let’s not catch the private colleges as the biggest family budget buster.
The Triple Aim
So, over the course of five articles, I have talked about how we as hospitalists have faced and learned about key aspects of delivering care in a modern healthcare system. First, it was economics, then patient safety and quality, then patient experience, and now we’re back to economics as we consider patient affordability.