Does U.S. Healthcare Need More Diverse Leadership?
Throughout its history, the United States has been a nation of immigrants. From the early colonial settlements to the mid-20th century, most immigrants came from Western European countries. Since 1965, when the Immigration and Nationality Act abolished national-origin quotas, the diversity of immigrants has increased. “By the year 2043,” says Tomás León, president and CEO of the Institute for Diversity in Health Management in Chicago, “we will be a country where the majority of our population is comprised of racial and ethnic minorities.”
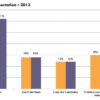
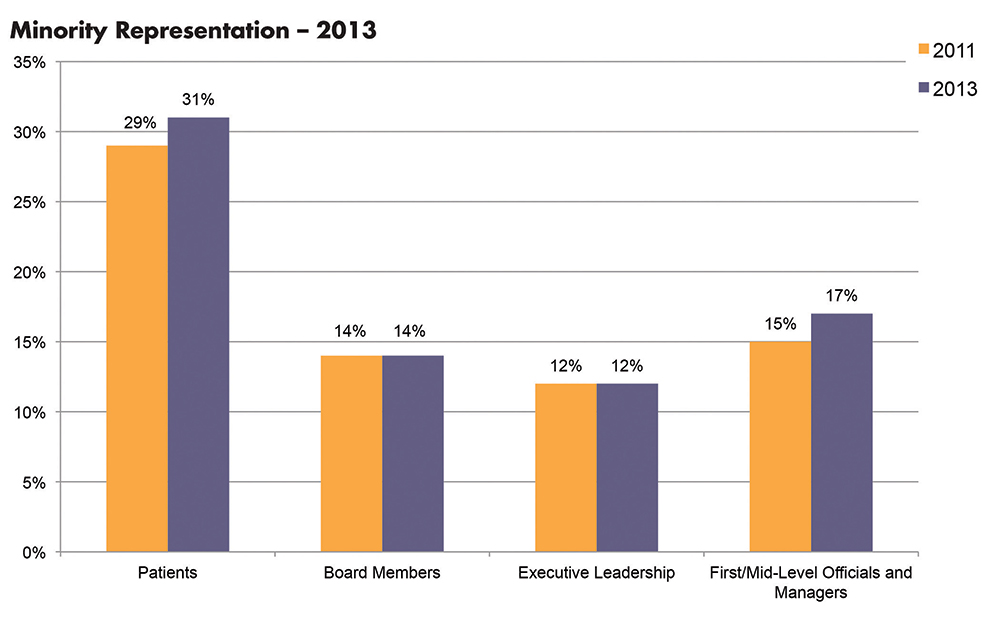
Those changing demographics, cited from the U.S. Census Bureau’s projections, already are evidenced in hospital patient populations. According to a benchmarking survey sponsored by the institute, which is an affiliate of the American Hospital Association, the percentage of minority patients seen in hospitals grew from 29% to 31% of patient census between 2011 and 2013.1 And yet, the survey found this increasing diversity is not currently reflected in leadership positions. During the same time period, underrepresented racial and ethnic minorities (UREM) on hospital boards of directors (14%) and in C-suite positions (14%) remained flat (see Figure 1).
Gender disparities in healthcare and academic leadership also have been slow to change. Periodic surveys conducted by the American College of Healthcare Executives indicate that women comprise only 11% of healthcare CEOs in the U.S.2 And despite the fact that women make up half of all medical students (and one-third of full-time faculty), the Association of American Medical Colleges (AAMC) finds that women still trail men when it comes to attaining full professorship and decanal positions at their academic institutions.3
The Hospitalist interviewed medical directors, researchers, diversity management professionals, and hospitalists to ascertain current solutions being pursued to narrow the gaps in leadership diversity.
Why Diversity in Leadership Matters
Eric E. Howell, MD, MHM, chief of the Division of Hospital Medicine at Johns Hopkins Bayview Medical Center in the Hopkins School of Medicine in Baltimore, believes there is a need to encourage the advancement to leadership positions for female and UREM physicians.
“In medicine, it’s really about service. If we are really here for our patients, we need representation of diversity in our faculty and leadership,” says Dr. Howell, a past SHM president and faculty member of SHM’s Leadership Academy since its inception in 2005. In addition, he says, “Diversity adds incredible strength to an organization and adds to the richness of the ideas and solutions to overcome challenging problems.”
With the implementation of the Affordable Care Act, formerly uninsured people are now accessing the healthcare system; many are bilingual and bicultural, notes George A. Zeppenfeldt-Cestero, president and CEO, Association of Hispanic Healthcare Executives.
“You want to make sure that providers, whether they are physicians, nurses, dentists, or health executives that drive policy issues, are also reflective of that population throughout the organization,” he says. “The real definition of diversity is making sure you have diversity in all layers of the workforce, including the C-suite.”
León points to the coming “seismic demographic shifts” and wonders if healthcare is ready to become more reflective of the communities it serves.
“Increasing diversity in healthcare leadership and governance is essential for the delivery and provision of culturally competent care,” León says. “Now, more than ever, it’s important that we collectively accelerate progress in this area.”
Advancing in Academic and Hospital Medicine
Might hospital medicine offer additional opportunities for women and minorities to advance into leadership positions? Hospitalist Flora Kisuule, MD, SFHM, assistant professor of medicine at Johns Hopkins School of Medicine and associate division director of the Collaborative Inpatient Medicine Service (CIMS) at Johns Hopkins Bayview Medical Center, believes this may be the case. She was with Dr. Howell’s group when he needed to fill the associate director position.