How hospitalists can help reduce readmissions
Hospital readmissions are frequent, harmful, and costly. Consider the fact that 18% of Medicare patients can expect to be readmitted within 30 days at a cost of more than $17 billion.1 Recent changes in health care policy aimed at reducing readmission have substantially increased attention to this major health care issue.2
The Affordable Care Act has mandated that the Centers for Medicare & Medicaid Services reduce payment to hospitals with higher-than-expected 30-day readmissions, with its Hospital Readmissions Reduction Program. This has driven rapid growth in the study of patients rehospitalized within 30 days of discharge.3 So what are some strategies that have either been proven to reduce readmissions or show promise in doing so?
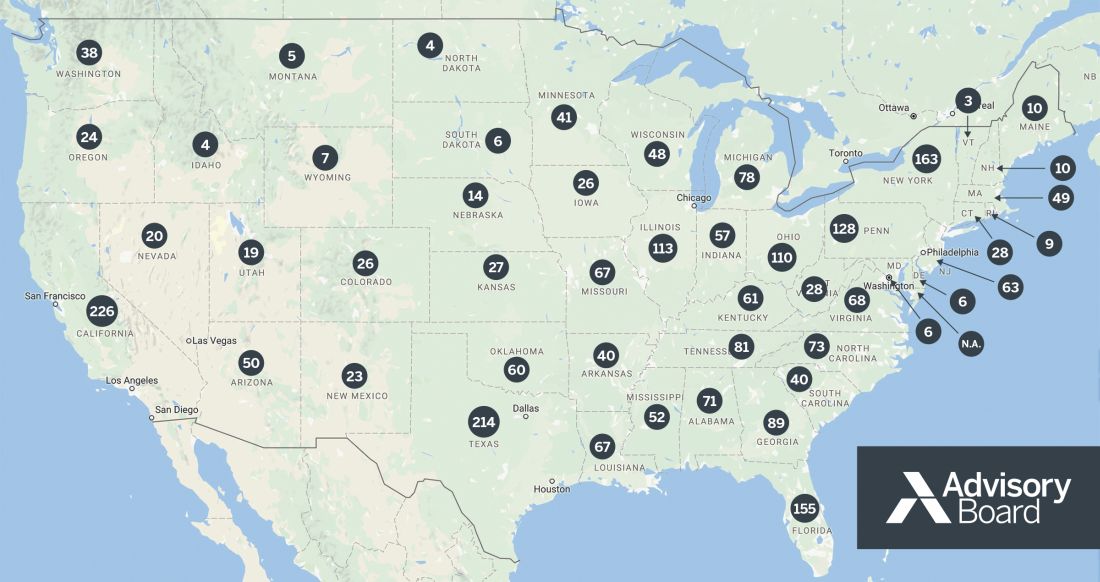
FY 2017 IPPS Final Rule HRRP Supplemental Data File. Courtesy of Advisory Board.
This map reflects the number of hospitals in each state that will receive a penalty in fiscal year 2017 under the Hospital Readmissions Reduction Program (HRRP). Performance reporting period for FY 2017 program year was July 1, 2012, to June 30, 2015.
An ounce of prevention
In studying inpatient and outpatient physicians’ perspectives regarding factors contributing to readmission,4 Shoshana Herzig, MD, MPH, assistant professor of medicine, Harvard Medical School, and director of Hospital Medicine Research, Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, and her colleagues identified some potential preventive strategies.
The most commonly endorsed strategy to prevent readmissions by both primary care physicians and hospitalists surveyed involved improving self-management plans at discharge. “This refers to actions such as providing patient-centered discharge instructions (that is, making sure they are written in language that patients can understand) or asking transition coaches to help facilitate a successful transition,” Dr. Herzig said. “This finding is consistent with the fact that the factor most commonly identified as contributing to readmissions was insufficient patient understanding or ability to self-manage. Combined, these findings suggest that strategies to enhance patient understanding of their illness, care plan, and what to expect after hospital discharge, are likely to be important components of successful readmission reduction programs.”
Another commonly endorsed strategy to prevent readmission was greater engagement of home and community supports. This entails enlisting the help of social workers and community agencies to deliver meals, provide transportation to doctors’ appointments, and so forth. “Inadequate social support contributes to many readmissions,” Dr. Herzig said. “Hospitalists should request assistance from social workers in helping to secure assistance for patients who need these services.”
Provisioning of resources to patients to help them manage their care after discharge is also recommended. For example, engaging nurses or pharmacists who can help with issues that arise after discharge may help keep patients out of the hospital.
“Hospitalists should be aware of what resources are available to help patients manage their care,” Dr. Herzig said. For example, if a patient needs periodic blood pressure monitoring, the hospitalist can tell the patient about free blood pressure checkpoints or suggest a home-automated blood pressure monitor.
The study also showed that improved coordination of care between inpatient and outpatient providers, such as sharing medical records, could reduce readmission rates. “This allows for better inpatient care and increased ability for primary care physicians to react appropriately to issues arising after discharge,” Dr. Herzig said. “In the absence of a shared system, hospitalists should complete discharge summaries in a timely fashion and ensure that they’re promptly transmitted to primary care physicians.”
Finally, the researchers believe that multifaceted, broadly applied interventions may be more successful than those relying upon individual providers choosing specific services based on perceived risk factors. “This is because a prior study5 demonstrated that it is difficult to anticipate in advance which patients will be readmitted, and, in our study, physicians did not agree on the factors that contributed to a given readmission,” Dr. Herzig explained. “Because of these findings, it becomes hard to rely on physicians to identify patients at increased risk for readmission, and to direct services that correctly anticipate contributing factors. Instead, it seems that programs aimed at improving general processes for particular patient categories may be more successful at reducing readmissions.” For example, it might be better to use a transition coach for all patients over the age of 65, rather than relying on physicians to decide which patients are at high risk for readmission.
Dr. Herzig said it’s important to note that hospitalists and primary care physicians had different appraisals of reasons for readmission. Therefore, when designing readmission reduction programs or determining specific services to prevent a readmission for a given patient, it is important for hospitalists to obtain input from primary care physicians to ensure that they address all of the potential contributors to readmission for a given patient.