Hospitals filling as flu season worsens
Through the last full week of January, the cumulative “hospitalization rate is the highest we’ve seen,” acting Centers for Disease Control and Prevention director Anne Schuchat, MD, said. For the current season so far, the hospitalization rate stands at 51.4 per 100,000 population, putting it on pace to top the total of 710,000 flu-related admissions that occurred during the 2014-2015 season, she said in a weekly briefing Feb. 2.
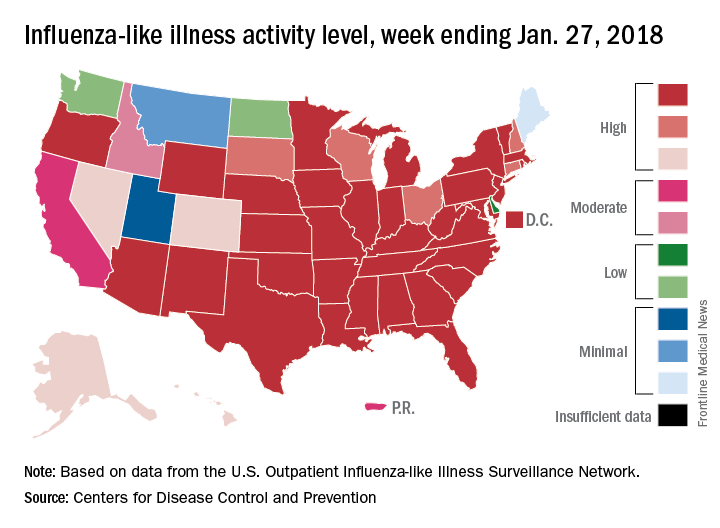
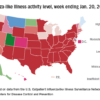
Stepping out of the hospital, the proportion of outpatient visits for influenza-like illness (ILI) was 7.1% for the week ending Jan. 27, which is up from 6.5% the previous week and continues to approach the all-time high of 7.7% set in the pandemic season of 2009-2010. ILI activity was at level 10 on the CDC’s 1-10 scale in 34 states, compared with 30 the week before, and was categorized in the “high” range (levels 8-10) in another 9 states, according to data from the CDC’s Outpatient Influenza-like Illness Surveillance Network.
Flu-related pediatric deaths also took a big jump for the week as another 16 were reported, which brings the total for the season to 53. Of the children who have died so far, only 20% were vaccinated, said Dan Jernigan, MD, MPH, director of the influenza division at the CDC’s National Center for Immunization and Respiratory Diseases, Atlanta. He also noted that half of the children who have been hospitalized did not had an underlying condition.
The one bit of good news for the week was that activity in the West seems to be easing up, Dr. Schuchat said. The geographic spread of ILI was reported as widespread in 48 states, which is down from 49 the previous week because Oregon dropped off the list. To go along with that, the ILI activity level in California has dropped 2 weeks in a row and now stands at level 7, the CDC data show.