
A 68-year-old man on chronic steroids for amiodarone-induced thyroiditis presented with pneumonia, hypotension, and encephalopathy. Though the pneumonia resolved, his encephalopathy worsened, and he became somnolent. Creatinine was 0.7 mg/dL (normal, 0.7 to 1.3 mg/dL) with an estimated glomerular filtration rate (eGFR) of 91 mL/min/1.73m². Cystatin C was 3.86 mg/L (normal 0.61 to 0.95 mg/L), and the recalculated eGFR, incorporating creatinine and cystatin C, was 29 mL/min/1.73m².
Brief Overview
Accurate assessment of glomerular filtration rate (GFR) is essential for diagnosing, staging, and managing acute and chronic kidney disease (CKD), determining medication dosages, and predicting outcomes such as CKD progression, cardiovascular events, and all-cause mortality.1 Although direct GFR measurement via exogenous clearance markers is the gold standard, it is costly and impractical for routine use.1
The most widely used method to estimate GFR is the 2021 creatinine-based chronic kidney disease epidemiology collaboration, or CKD-EPI, equation. Creatinine, a byproduct of muscle metabolism, is filtered and excreted by the kidneys.1 However, its levels are strongly influenced by muscle mass, diet, age, sex, and chronic illnesses such as advanced heart failure or cirrhosis.2 Laboratory measurements of creatinine can also be affected by elevated bilirubin, ketones, severe hyperglycemia, and severe acidosis.3
Creatinine levels tend to increase after age 70.1,2 Men generally have higher levels due to greater muscle mass, leading to increased creatinine production.1,2 Commonly used medications such as anti-retroviral medications for human immunodeficiency virus, H2 blockers, and trimethoprim/sulfamethoxazole inhibit tubular creatinine secretion and artificially raise creatinine levels, leading to an underestimation of glomerular filtration.2 Conversely, in sarcopenic patients, low muscle mass falsely lowers creatinine levels, leading to an overestimation of kidney function. Other factors frequently encountered by hospitalists, such as fluid overload, liver and heart disease, and dietary variability in meat consumption, also lead to GFR overestimation.1,2 Additionally, creatinine is not reliable for identifying early kidney disease due to limitations in sensitivity and specificity. It can take 24 to 48 hours to rise after an initial insult, delaying recognition of acute kidney injury.1
Overview of the Data
Cystatin C has emerged as a valuable additional biomarker for estimating GFR. It is a 13-kilodalton protein produced by all nucleated cells and freely filtered by the glomerulus.2 Unlike creatinine, cystatin C is unaffected by muscle mass or dietary intake, making it a more accurate and reliable measure of kidney function.1
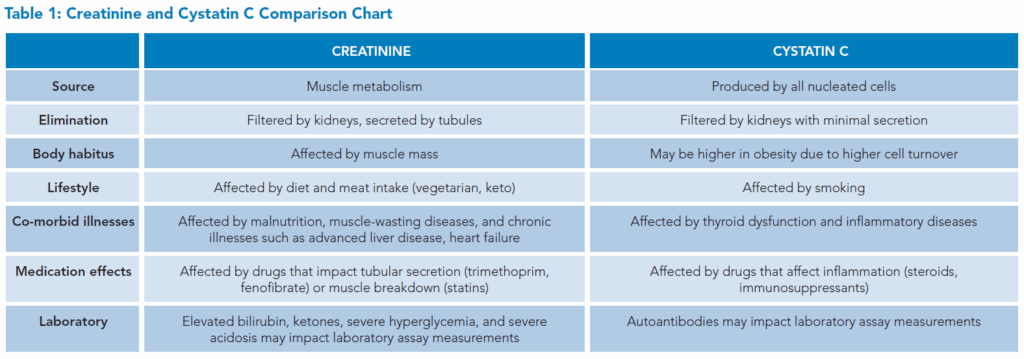
In both inpatient and outpatient settings, cystatin C has shown increased sensitivity to early changes in kidney function when compared to creatinine and has been used for early detection of both acute and chronic kidney disease.2,4 It also provides a more accurate assessment of the true kidney function, especially in populations where muscle metabolism is affected, such as patients with limb amputations, significant muscle atrophy, or altered muscle metabolism.2,5 This improved accuracy becomes even more pronounced in acutely ill patients, where creatinine production is often unpredictable and variable.6 Current guidelines recommend the use of cystatin C in conjunction with creatinine for more accurate GFR estimation in these populations. 3 See Table 1 for a detailed comparison of the two biomarkers.
 Common hospital medications with a narrow therapeutic window, including vancomycin, can be more accurately dosed when using cystatin C versus creatinine.2,5,6 Cystatin C is not affected by medications that inhibit tubular secretion of creatinine, providing a more accurate eGFR than creatinine.2
Common hospital medications with a narrow therapeutic window, including vancomycin, can be more accurately dosed when using cystatin C versus creatinine.2,5,6 Cystatin C is not affected by medications that inhibit tubular secretion of creatinine, providing a more accurate eGFR than creatinine.2
Limitations
Although cystatin C usage is becoming more prevalent, it is not performed internally at all hospitals, which increases cost and delays results. Cystatin C has wider interlaboratory variability than creatinine, affecting its use when comparing across health systems. However, as cystatin C availability and use increase, variability and cost are expected to decrease.2,5,6
For example, at our institution, cystatin C is now processed in-house, facilitating turnaround times that are comparable to those for serum creatinine.
Both creatinine and cystatin C can be affected by various factors, although cystatin C levels appear to be affected by fewer factors and to a lesser degree compared to creatinine.2 In general, conditions and medications that lead to increased cell turnover can elevate cystatin C, leading to an underestimation of GFR.2 Glucocorticoids and immunosuppressants, as well as states with high cell turnover such as malignancy, inflammatory disease, smoking, and obesity, may falsely increase cystatin C levels.1,2,7 Thyroid dysfunction can also affect cystatin C levels. Hyperthyroidism increases cystatin C, and hypothyroidism lowers cystatin C due to the stimulatory effects of thyroid hormone on cystatin C production.2,8 Additionally, laboratories that use immunoassay techniques may be affected by the presence of autoantibodies in autoimmune conditions, potentially interfering with assay binding.
How to Use Cystatin C in Your Daily Practice
The eGFRcr-cys equation, which incorporates both creatinine and cystatin C, provides a more accurate and precise assessment of renal function than using either biomarker alone.¹ Current guidelines recommend adding cystatin C to creatinine-based estimates when the creatinine-only eGFR is suspected to be inaccurate. This is particularly relevant in situations where creatinine levels may be influenced by factors such as muscle mass, diet, age, sex, disease states, or medications.¹⁻³ Using both markers together improves diagnostic confidence and supports more informed clinical decision-making.
Cystatin C obtained early in a patient’s hospitalization may lead to more timely identification of acute kidney injury.4,5 Creatinine lags in the identification of changes; therefore, the addition of cystatin C can provide earlier recognition of changes in kidney function.1,4,5 Incorporating cystatin C into the eGFR calculation can improve accuracy in patients who have muscle atrophy, limb amputation, prolonged immobilization, liver disease, protein-calorie malnutrition, spinal cord injury, or acute illness, since creatinine alone can be inaccurate.6 Additionally, obtaining a cystatin C can improve the eGFR calculation compared to creatinine alone and better guide appropriate medication dosing and avoid toxicity when using a medication with a narrow therapeutic window.2,5,6 It is important to emphasize that cystatin C and creatinine tests are independent and should not be used interchangeably or directly compared.
Application of Data to Case
The patient has multiple factors that could impact both cystatin C and creatinine measurements, including chronic low-dose steroid use, profoundly low muscle mass, and prior thyroid dysfunction. The combined creatinine-cystatin eGFR calculation provides a more accurate representation of his kidney function, revealing a much lower eGFR and exposing cefepime-induced neurotoxicity as the etiology of his ongoing encephalopathy.
Bottom Line
Cystatin C is a reliable biomarker that complements creatinine in estimating eGFR, leading to a more timely and accurate assessment of kidney function. When used alongside creatinine, it enhances both diagnostic and prognostic accuracy—especially in populations where creatinine alone may be less reliable.

Dr. Signoff

Dr. Kapa

Dr. Shi
Dr. Signoff is an adult hospitalist and an associate professor at the University of California, Davis in Sacramento, Calif. Dr. Kapa is an adult nephrologist and an assistant professor at the University of California, Davis in Sacramento, Calif. Dr. Shi is an adult hospitalist and an assistant professor at the University of California, Davis in Sacramento, Calif.
Quiz
1. A 75-year-old woman with a history of poorly controlled diabetes, prior left above-the-knee amputation, and severe protein-calorie malnutrition is admitted for right lower extremity cellulitis. Her serum creatinine is 0.5 mg/dL, corresponding to an eGFR of 105 mL/min/1.73m². However, her cystatin C level is significantly elevated, and her combined eGFR using cystatin C and creatinine is 40 mL/min/1.73m². What is the most likely reason for the discrepancy?
a. Overestimation of kidney function by creatinine due to amputation history
b. Underestimation of kidney function by cystatin C due to poorly controlled diabetes
c. Interlaboratory variability of cystatin C assay measurement
d. Hyperglycemia interfering with cystatin C assay
Correct Answer: a. Patients with severe malnutrition or lower muscle mass due to amputations may produce less creatinine, leading to an overestimated eGFR. Cystatin C, which is independent of muscle mass, provides a more accurate measure of kidney function in such patients, revealing significant kidney dysfunction that might otherwise be missed. While inflammatory conditions may falsely increase cystatin C, leading to an underestimation of eGFR, poorly controlled diabetes has not been seen to have this effect. Interlaboratory variability may impact the ability to directly compare cystatin C levels between institutions, but would not explain the discrepancy between eGFR calculations here. Hyperglycemia can interfere with creatinine assay measurements, but cystatin C assays are not similarly affected.
References
1. Inker LA, Titan S. Measurement and estimation of GFR for use in clinical practice: core curriculum 2021. Am J Kidney Dis. 2021;78(5):736-749. doi:10.1053/j.ajkd.2021.04.016.
2. Chen DC, et al. Advantages, limitations, and clinical considerations in using cystatin C to estimate GFR. Kidney360. 2022;3(10):1807-1814. doi:10.34067/KID.0003202022.
3. Kidney disease: improving global outcomes (KDIGO) CKD work group. KDIGO 2024 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int.2024;105(4S):S117-S314. doi:10.1016/j.kint.2023.10.018.
4. Soto K, et al. Cystatin C as a marker of acute kidney injury in the emergency department. Clin J Am Soc Nephrol. 2010;5(10):1745-1754. doi:10.2215/CJN.00690110.
5. Lees JS, et al. Cystatin C should be routinely available for estimating kidney function. Curr Opin Nephrol Hypertens. 2024;33(3):337-343. doi:10.1097/MNH.0000000000000980.
6. Ebert N, Shlipak MG. Cystatin C is ready for clinical use. Curr Opin Nephrol Hypertens. 2020;29(6):591-598. doi:10.1097/MNH.0000000000000638.
7. Bjarnadóttir M, et al. Promoter-mediated, dexamethasone-induced increase in cystatin C production by HeLa cells. Scand J Clin Lab Invest. 1995;55(7):617-623.doi:10.3109/00365519509110261.
8. Schmid C, et al. Triiodothyronine stimulates cystatin C production in bone cells. Biochem Biophys Res Commun. 2012;419(2):425-430. doi:10.1016/j.bbrc.2012.02.040.