 A 64-year-old female is admitted to the hospital with pneumonia and started on IV antibiotics. You see her after she has been admitted and start some IV fluids for presumed sepsis. On day two, the patient improves, and you are asked by your institutional coder to clarify whether this patient truly has sepsis and to document it accordingly.
A 64-year-old female is admitted to the hospital with pneumonia and started on IV antibiotics. You see her after she has been admitted and start some IV fluids for presumed sepsis. On day two, the patient improves, and you are asked by your institutional coder to clarify whether this patient truly has sepsis and to document it accordingly.
What documentation is necessary for sepsis?
Sepsis can safely be documented using the Sepsis-3 criteria from the third international consensus definitions for sepsis and septic shock (2016) that requires the acute change in SOFA score of >2 from baseline consequent to a recognized infection. This represents a dysregulated response of organ systems to an infection.
Tip
For clinical validation purposes, your clinical documentation improvement specialist might be looking for documentation that:
- Demonstrates the presence of infection, whether the source is known or unknown
- Has evidence of organ dysfunction demonstrating an increase of two or more points in the SOFA score
- Shows organ dysfunction, usually in more than one organ system (e.g., an elevated creatinine level resulting in a SOFA score of 3 by itself is less supportive of clinically validating sepsis)
- Indicates treatment directed at the underlying source of the sepsis and directed at the clinical consequences of the sepsis (e.g., acute kidney injury, respiratory failure, etc.)
Dr. Mehta is the vice-chair of inpatient clinical affairs, medical director, and assistant professor of medicine in the clinical core faculty for program valuation and improvement at the University of Cincinnati Medical Center in Cincinnati.
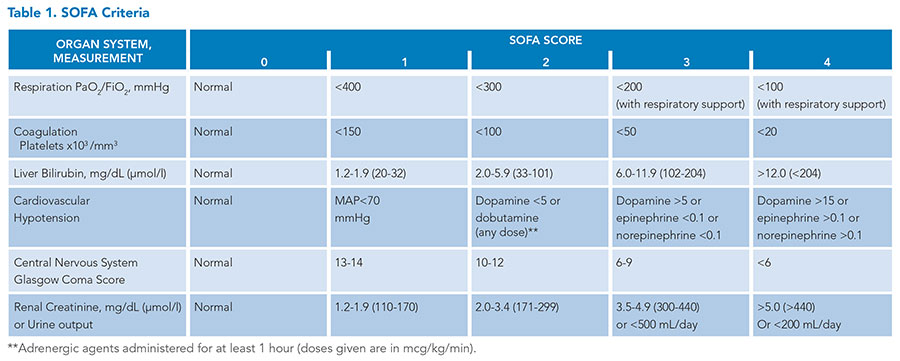
The SOFA-3 criteria were validated for adult patients and not for pediatric patients. For example, in the case presented, an abnormal creatinine level would be much lower than the threshold 1.2 to earn 1 point for the renal component due to the age of the patient and age-variable norms in pediatrics. The Phoenix criteria, published in January 2024, should be used when addressing the diagnosis of sepsis in pediatric patients (<18y).
Apologies for the misprint. It was supposed to be a 64- year old lady, not 4 year old. It was typed correctly in print but not in the online version. I will look to try to correct this.