The Pathophysiology of Preeclampsia
Based on this observation of normal pregnancy, the following three lines of investigation have furthered our understanding of the potential pathophysiology of pre-eclampsia.
1. Because NO appears to play an important role in the normal vasodilation of pregnancy, abnormalities in this vascular regulatory pathway may be critical to the development of hypertension. Asymmetric dimethylarginine (ADMA) competitively inhibits NO production from arginine by nitric oxide synthetase (NOS). Savvidou and colleagues showed that women with ultrasound evidence of low uterine blood flow were more likely to develop preeclampsia and exhibited higher ADMA levels.11 There was a strong inverse relationship between ADMA levels and flow-mediated vasodilation in women who developed preeclampsia.
Similarly, dimethylarginine dimethylaminohydrolase (DDAH II), an enzyme that metabolizes ADMA, is strongly expressed in placental tissue. In states of placental insufficiency, one might speculate that levels of DDAH II would be reduced, while ADMA levels would increase. Along this same line of investigation, Noris and colleagues have shown increased arginase II activity in placental tissue from preeclamptic individuals and subsequently reduced levels of L-arginine, a substrate for NO production.12
2. A second line of promising research involves the production of a circulating inhibitor of VEGF. The growth factors VEGF and PlGF are produced by the placenta and affect vascular function by binding to two high affinity receptor tyrosine kinases: kinase insert domain-containing region (KDR) and Fms-like tyrosine kinase 1 receptor (Flt-1). Alternative splicing results in the production of an endogenously secreted protein, soluble Fms-like tyrosine kinase 1 receptor (sFlt-1), which lacks the transmembrane and cytoplasmic region of the VEGF receptor and cannot become membrane bound, but that binds VEGF and PlGF. Once VEGF has bound to sFlt-1, normal binding to the membrane-bound receptor is inhibited; thus the effects of VEGF are inhibited.
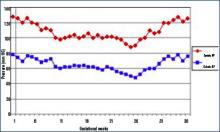
Studies have found that infusion of sFlt-1 to nonpregnant animals causes glomerular endotheliosis and hypertension similar to those found in preeclampsia; these findings support the possibility that sFlt-1 contributes to preeclampsia. Further, Levine and colleagues have shown that plasma sFlt-1 levels increase more in women with preeclampsia and precede clinical findings compared with individuals with normal pregnancies.13 In addition, PlGF levels were decreased in women with preeclampsia compared with the levels found in those experiencing normal pregnancies.
The supposition from these studies is that increased plasma levels of sFlt-1 competitively inhibit VEGF binding to VEGF receptors on vascular tissue. This inhibition causes a lack of vasodilation and increased blood pressure, with the normal fluid retention and volume expansion of pregnancy. VEGF is difficult to accurately determine in plasma, but PlGF levels, which are affected similarly, are reduced in individuals suffering from or destined to develop preeclampsia. Furthermore, since VEGF is an important determinant of normal placental development, decreased cellular binding due to competitive inhibition could contribute to abnormal placental pseudovasculogenesis.
3. Finally, Vu and colleagues have shown that pregnant animals made hypertensive by a high salt diet and deoxycorticosterone administration exhibit a higher circulating level of the Na, K-ATPase inhibitor, marinobufagenin.14 Further, blood pressure is reduced by the administration of the inhibitor of this cardenolide compound, resibufogenin. Though this is not a model of spontaneous preeclampsia, many features are similar, including reduced placental blood flow in spite of volume expansion and proteinuria.
Treatment Recommendations
1. In individuals with hypertension prior to pregnancy, the physician may continue the same anti-hypertensive therapy used pre-pregnancy, with or without diuretics—except for angiotensin-converting enzyme inhibitors or angiotensin receptor blockers. The goal is to maintain the blood pressure at or below a level of 140/90 mm Hg. The pregnancy should be monitored as a high-risk pregnancy, and urine protein excretion, blood pressure, and fetal health should be monitored frequently, particularly after the 24th week of gestation. Urine protein excretion is most easily monitored using a spot urine protein-to-creatinine ratio. A value of less than 0.3 is equivalent to a 24-hour urine excretion of less than 300 mg.