Phuoc Le, MD, MPH, was born a year after the Vietnam War ended and was five when he and his family fled Vietnam by boat to seek asylum in Hong Kong. At a refugee camp there, he had his first contact with a functional public health system and, within days, was cured of the parasitic disease that had made him ill since he was a toddler. Later, as an undergraduate at Dartmouth College in Hanover, N.H., he realized he had been one of the health disparity victims described by medical anthropologist Paul E. Farmer, PhD, MD, in his books.
“For the vast majority of people, it doesn’t turn out the way it did for me,” says Dr. Le. “As much as I’ve been blessed with, what I expect of myself is to focus on health disparities and have it be my life’s work.”
Dr. Le’s personal mission led him to co-found the Global Health Core within the division of hospital medicine at the University of California San Francisco, which aims to train hospitalists to work in resource-poor settings. The program recently was honored with the 2015 SHM Award for Excellence in Humanitarian Service.
Dr. Le, assistant professor of medicine and pediatrics at the University of California San Francisco (UCSF), where he co-directs the Global Health-Hospital Medicine Fellowship, recently spoke with The Hospitalist about his work.
Question: What was your first trip as a physician abroad like?
Answer: I was a resident at Harvard [University in Cambridge, Mass.] in 2007 when I went to Haiti with Paul Farmer and a few other residents involved in the [nonprofit] Partners in Health. I’ll never forget that the trip from Port-au-Prince to the hospital was only about 120 miles, and it took eight hours in a four-wheel drive vehicle to get there. They didn’t want us residents to suffer that trip, so they got a bunch of volunteer pilots to fly us in a single-engine plane, which took about 20 minutes.
We got there, had lunch and dinner, and it was during dinner that the group coming by vehicle finally arrived. It just dawned on me. These are things you don’t have a visceral feeling for until you see them. These people were tired because they had driven all day. What if I had been a patient and had to travel 120 miles and was sick? Would I have lasted eight hours to go that small distance?
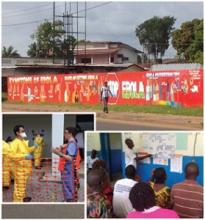
This is just one example of many structural problems that need to be addressed. The same conditions are impeding the progress in [controlling] Ebola in West Africa. I was there in November. The problems that led to [the] Ebola [outbreak] were absolutely predictable and avoidable if the global community had paid more attention to this injustice before Ebola started—or responded much earlier. It could have saved lives [and] money, and we probably wouldn’t have had the huge scare in the U.S. that we did.
Q: What compelled you to go to Liberia just as the Ebola outbreak began?
A: To me, there was no question in my mind that I needed to go. It was a situation where I had the expertise. I’m a physician, a public health expert, [I’ve] worked in places with tropical diseases and have experience responding to emergencies like the cholera epidemic in Haiti and the Haiti earthquake. We also had a relationship with an NGO [non-governmental organization] in Liberia for several years. My colleagues and I at UCSF started the nation’s first global health hospital medicine fellowship, and our fellows had been going to Liberia for the last three years. For us, it was a matter of solidarity.