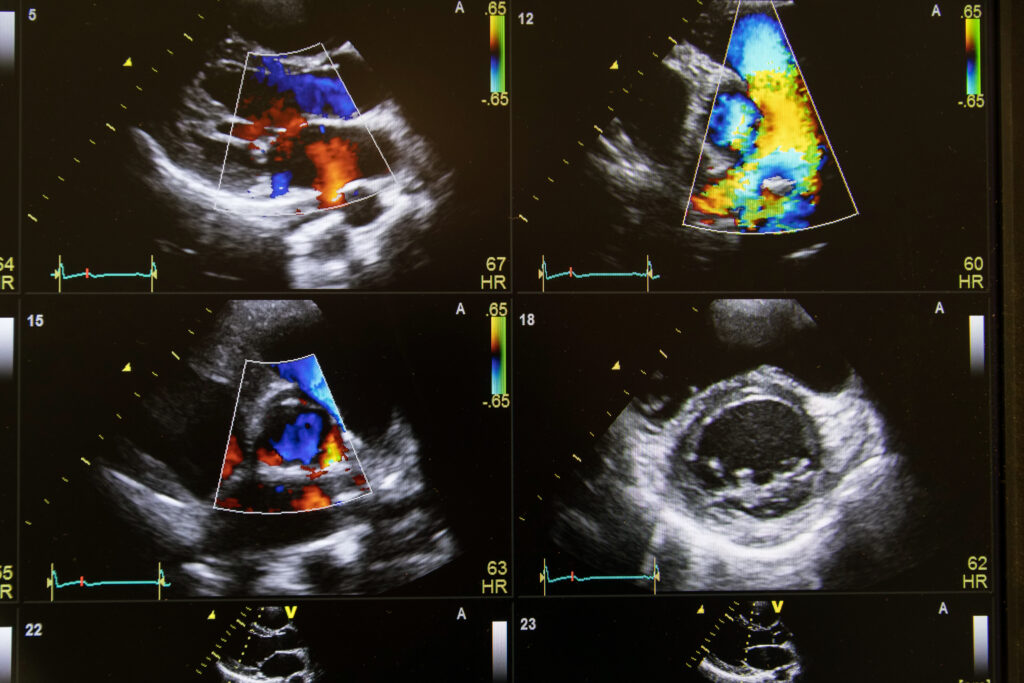
Heart ultrasound image on a computer screen.
In many hospitals across the nation, hospitalists assume leadership roles during rapid response and code blue events, especially in settings where immediate critical care support is limited.1 Point-of-care ultrasound (POCUS) has become an invaluable extension to the physical exam in cardiac patient assessment, especially in these high-acuity moments, where patients are too unstable to be transferred to a CT scan or too sick to wait for a formal echocardiogram study to be done.2 POCUS is used as a handy, efficient, and safe tool that allows the assessment of left and right ventricular function, detection of pericardial effusion, and estimation of intravascular volume status.3
POCUS plays a critical role in the bedside differentiation of shock or near-shock states, enabling more targeted and timely resuscitation with the additional potential to allow dynamic evaluation of volume responsiveness.4
Additionally, in the context of newly detected prominent cardiac murmurs, a focused echocardiogram can provide live visual evidence of significant valvular abnormalities such as regurgitation or stenosis, influencing medication choice and prompting expedited
consultation and intervention.
While complete echocardiography includes multiple views, internists can gather the essential information relevant to their scope of practice using just four core cardiac windows:
- Parasternal long-axis (PLAX)—best for left ventricular (LV) systolic function, pericardial effusion, and aortic root assessment
- Parasternal short-axis (PSAX)—best for assessing regional wall motion abnormalities and right ventricular (RV) pressure or volume overload
- Apical four-chamber (A4C)—best for comparing LV and RV size and function, assessing pericardial effusion, valve regurgitation,
and aortic velocity-time integral (VTI), which helps assess LV function - Subcostal four-chamber view—to obtain limited views in critically ill patients or those with emphysema as an excellent alternative when other views are suboptimal; also useful for evaluating pericardial effusion
Introducing the “Pump–Tank–Leaks” framework as a structured approach to cardiac assessment provides a practical and intuitive model for hemodynamic evaluation at the bedside. “Pump” refers to the evaluation of cardiac function, “Tank” pertains to the assessment of volume status, and “Leaks” focuses on the evaluation of valvular integrity and function.
LV Assessment
Case: A 72-year-old man undergoing chemotherapy for cancer presented with nausea and progressive shortness of breath. He was noted to be mildly hypotensive on presentation with a lactic acid level of 5 mmol/L. Physical examination revealed overall clear lungs bilaterally, without clear signs of volume overload or jugular vein distention, making the etiology of his dyspnea unclear. Bedside POCUS using the PLAX view demonstrated a markedly reduced left ventricular ejection fraction with globally diminished contractility. No clear, focal, wall motion abnormality was appreciated on the parasternal short-axis view. The B-type natriuretic peptide was elevated at 920 pg/mL, and troponins were mildly positive, consistent with newly diagnosed heart failure. While IV fluid administration is often the initial intervention for hypotensive patients, in this case, it could have exacerbated the patient’s condition. IV fluids were withheld, cardiology was consulted, and the patient was admitted to the cardiac intensive care unit for a milrinone drip. A comprehensive workup for cardiomyopathy was initiated, and after ischemic etiologies were excluded, the patient was diagnosed with chemotherapy-induced cardiomyopathy. Guideline-directed medical therapy was initiated, and the patient was discharged home one week later.
Clinical pearl: A quick eyeball assessment of LV contractility helps differentiate heart failure from other causes of dyspnea. Visual estimation is often enough to change management when time matters.5,6
RV Assessment
Case: A 55-year-old woman presented with syncope, tachycardia, and mild hypotension. The ECG did not reveal acute changes besides sinus tachycardia. POCUS shows an enlarged RV with septal flattening, also known as the D sign, on PSAX view. Interestingly, POCUS also noted McConnell’s sign, which is described in literature as a highly specific sign for pulmonary embolism and suggestive of right heart strain. The patient underwent CT angiography and was diagnosed with a massive pulmonary embolism. While IV fluid administration often is elected as a first intervention for patients with hypotension, it could have worsened the patient’s condition and applied more pressure on a weak RV.
Clinical pearl: RV enlargement and septal flattening are key signs of acute pulmonary embolism, with McConnell’s sign as a very specific finding.7
Pericardial Effusion and Tamponade
Case: A dialysis patient presented to the emergency department (ED) for shortness of breath and was found to be in acute hypoxic respiratory failure requiring BiPAP, with tachycardia, hypotension, and lactate of 4 mmol/L on labs. Bedside POCUS was performed. PLAX view could not reveal clear views of the heart due to non-invasive positive pressure ventilation and patient agitation due to subjective shortness of breath. The subcostal view was attempted and showed a large pericardial effusion with right atrial collapse. Cardiology was urgently called. Pericardiocentesis was performed and led to immediate hemodynamic stability.
Clinical pearl: Cardiac tamponade is a diagnosis not to miss. Bedside POCUS can expose it in seconds. Look for pericardial effusion and chamber collapse (atrial collapse during systole, ventricular collapse during diastole).8 Note that patients with pulmonary hypertension can have late chamber collapse even in the presence of tamponade, due to higher baseline chamber pressures.9
Volume Assessment
Case: A 64-year-old woman with pneumonia and hypotension was initiated on IV fluids in the ED and admitted to the floor for sepsis. After blood pressure initially improved, the patient had recurrent hypotension on the floor. The medicine team considered an ICU transfer for initiation of pressors, as they were nervous about giving more IV fluids since the patient received a full sepsis bolus in the ED. The patient was already requiring six liters per minute of oxygen support due to her pneumonia, and any degree of volume overload could put the patient in a worsening respiratory failure, warranting immediate ICU transfer. Bedside POCUS was performed, revealing the left ventricle (LV) to be hyperdynamic and underfilled, accompanied by a collapsed inferior vena cava (IVC) and more than 50% respiratory variation in IVC diameter. One more liter of IV fluid was ordered, which helped achieve optimal resuscitation and achieved the “stress volume” that resulted in hemodynamic stability and better perfusion and helped the patient avoid an unnecessary ICU admission.
Clinical pearl: Combined LV function with IVC assessment can guide fluid resuscitation. In the absence of certain exceptions, a collapsing IVC plus a small hyperdynamic LV suggests hypovolemia.10
Gross Valve Abnormalities
Case: A 68-year-old man with a history of hypertension presented to the ED for syncope earlier that evening while he was going upstairs. The patient was found to be mildly hypotensive in the ED with a narrow pulse pressure. Initial suspicion was dehydration, and IV fluids were considered. A careful bedside exam was performed and revealed a systolic murmur in the right upper sternal border that was never documented in the chart. PLAX view was performed and revealed a thickened and minimally mobile aortic valve, consistent with severe aortic stenosis with resulting LV outflow obstruction. Cardiology was consulted, and the patient was admitted for a transcatheter aortic valve replacement the next morning. IVF could have worsened the patient’s condition by potentially exacerbating pulmonary edema in the setting of severe aortic stenosis, resulting in decreased cardiac output.
Clinical pearl: While detailed valve assessment requires formal echo, some easy-to-find yet critical valvular problems can be detected on simple bedside POCUS, influencing the treatment plan and potentially avoiding harm.11
Summary
Integrating POCUS into cardiac patient assessment has transformed hospital care. Its use provides immediate bedside insights into cardiac function, enabling rapid, informed decisions that improve patient outcomes. POCUS also helps in diagnosing conditions like heart failure and guides appropriate interventions, enhancing patient care.

Dr. Abou Asala
Dr. Abou Asala is a hospitalist and associate staff physician in the department of hospital medicine of the Cleveland Clinic Foundation, and clinical assistant professor of medicine at the Cleveland Clinic Lerner College of Medicine, both in Cleveland.
References
1. DeGroot D, Callis A. Role delineation of the code blue team: a quasi-experimental study during COVID-19. J Emerg Nurs. 2023;49(2):287-293. doi: 10.1016/j.jen.2022.11.013.
2. Milne J, et al. sonography in hypotension and cardiac arrest (SHoC): rates of abnormal findings in undifferentiated hypotension and during cardiac arrest as a basis for consensus on a hierarchical point of care ultrasound protocol. Cureus. 2016;8(4):e564. doi: 10.7759/cureus.564.
3. Bhagra A, et al. Point-of-care ultrasonography for primary care physicians and general internists. Mayo Clin Proc. 2016;91(12):1811-1827. doi: 10.1016/j.mayocp.2016.08.023.
4. Argaiz ER, et al. Comprehensive assessment of fluid status by point-of-care ultrasonography. Kidney360. 2021;2(8):1326-1338. doi: 10.34067/KID.0006482020.
5. Maxwell AG, Jardine DL. Introduction of portable bedside echocardiography to acute general medicine. Intern Med J. 2019;49(8):1025-1028. doi: 10.1111/imj.14383.
6. Hathaway QA, et al. Ultrasonic texture features for assessing cardiac remodeling and dysfunction. J Am Coll Cardiol. 2022;80(23):2187-2201. doi: 10.1016/j.jacc.2022.09.036.
7. Salame G, Liu G. Basic cardiac point-of-care ultrasound and its clinical applications. Med Clin North Am. 2025;109(1):63-79. doi:10.1016/j.mcna.2024.07.008.
8. Alerhand S, et al. Pericardial tamponade: a comprehensive emergency medicine and echocardiography review. Am J Emerg Med. 2022;58:159-174. doi:10.1016/j.ajem.2022.05.001.
9. Khan MU, Khouzam RN. Protective effect of pulmonary hypertension against right-sided tamponade in pericardial effusion. South Med J. 2015;108(1):46-8. doi:10.14423/SMJ.0000000000000230.
10. Orso D, et al. Accuracy of the caval index and the expiratory diameter of the inferior vena cava for the diagnosis of dehydration in elderly. J Ultrasound. 2016;19(3):203-9. doi: 10.1007/s40477-016-0200-y.
11. Riera A, et al. Quantitative valve motion assessment in adolescents using point-of-care ultrasound: short communication. Ultrasound J. 2025;17(1):11. doi: 10.1186/s13089-025-00402-y.
