No matter on which side of the aisle you sit, and even if you’d prefer to just sit in your car and check Instagram, the results of the November election were likely a surprise. Speculation abounds by pundits and so-called experts as to what a Trump presidency means for health care in this country. The shape and scope of health care initiatives that a Trump administration will attempt to advance in place of the Affordable Care Act (ACA), which has likely met its demise, is unknown at the time of this writing. How Trump’s new initiatives fare in Congress and then get translated into practical changes in health care delivery and financing is even more muddled.
The U.S. medical community has remained largely silent, which is wise given the lack of evidence that would support any rational prediction, but perhaps it’s easier to pronounce judgment from across the pond. The Lancet recently reported the comment of Sophie Harman, PhD, a political scientist at Queen Mary University in London, who told an audience at the London School of Hygiene & Tropical Medicine to “ignore the dead cat in the room.”1 I spent 6 months of my residency in the United Kingdom, and this phrase never came up in my travels across the wards, streets, and pubs of the mother country. Apparently, the “dead cat strategy” is a legislative maneuver to distract attention from a party’s political shortcomings by raising a ruckus about a salacious or social hot-button topic. In this case, the dead cat may just be the carcass of Obamacare, exuding the fetor of millions of people losing their health insurance.
The BMJ, another respected U.K. journal, offered the pronouncement by Don Berwick, MD, former administrator of the Centers for Medicare & Medicaid Services, that Trump’s election would be “disastrous” for U.S. health care, but not much else.2
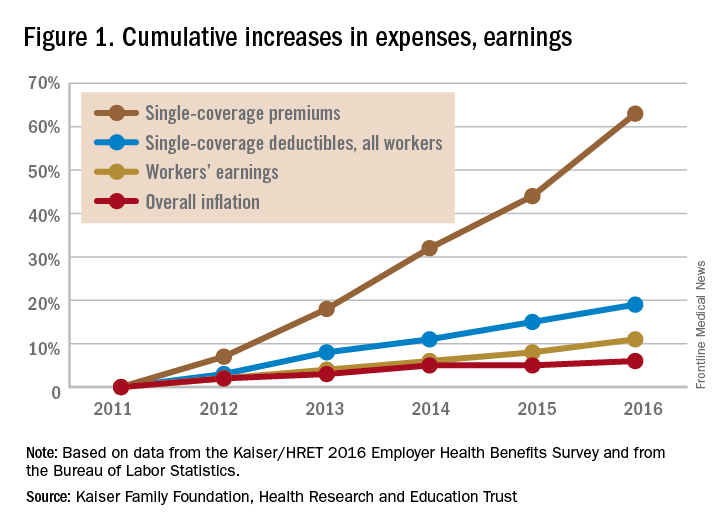
Whatever @realDonaldTrump has in mind, the truth not publicized by either party is that the drift of health care costs to patients and families, even amongst the insured, has already been killing household budgets. It has happened via a thousand cuts, in the form of increasing copays and deductibles, and is likely to get worse. Twenty million Americans gained insurance through either Medicaid expansion or subsidized health insurance as a result of ACA, which led to an overall reduction in out-of-pocket costs for Americans on the whole.3 But the pain of out-of-pocket costs spiked in certain situations: Average deductibles for covered employees were $1,478 in 2016, up 12% from 2015 and 49% compared to 2011.4Single-coverage deductibles over this period of time rose cumulatively by 63%.
Out-of-pocket health care expenses for patients and families insured under Medicaid and its ACA-mandated expansion decreased to, on average, less than $500 per year; however, 19 states, all with Republican governors, blocked the Medicaid expansion.5 This denied more than 2.5 million people Medicaid coverage in these states; the overwhelming majority of these people remained uninsured. Uninsured people incur significant out-of-pocket costs when they do require health care, and have worse outcomes.6,7 The end of ACA throws Medicaid expansion in any state, with its protections to limit out-of-pocket expenses, into doubt.
Before the ACA expanded Medicaid coverage, patients faced significant wait times and travel costs associated with the low numbers of providers accepting Medicaid’s low reimbursement rate.8 These numbers had begun to improve after the ACA increased primary care physicians’ Medicaid reimbursements to Medicare rates in 2013 and 2014, but only a limited number of states will continue the increases after the end of federal subsidies.
For people who purchased plans on the ACA’s marketplace, out-of-pocket exposure is capped in 2017 at no more than $7,150 for an individual plan and $14,300 for a family plan before marketplace subsidies. Even those who qualified for cost-sharing deductions, with incomes between 100% and 250% of the federal poverty level, had out-of-pocket caps that varied widely depending on plan and state. For example, in 2016 at the $17,000 annual income level, out-of-pocket caps could range from $500 to $2,250.9
Clinician concern
On a provider level, incentives to reduce readmissions and limit health care–associated harm events mandated by the ACA may soon evaporate, throwing into question many quality metrics pursued by health systems. In response, will health system administrators abandon efforts to reduce readmissions and hospital-acquired conditions (HACs)? Or will health systems, despite the lack of a Medicare penalty “stick,” move forward with efforts to reduce readmissions and HACs? There’s no question of what would benefit the pocketbooks of our patients the most – every hospitalization results in significant direct out-of-pocket costs, not to mention lost productivity and income.10