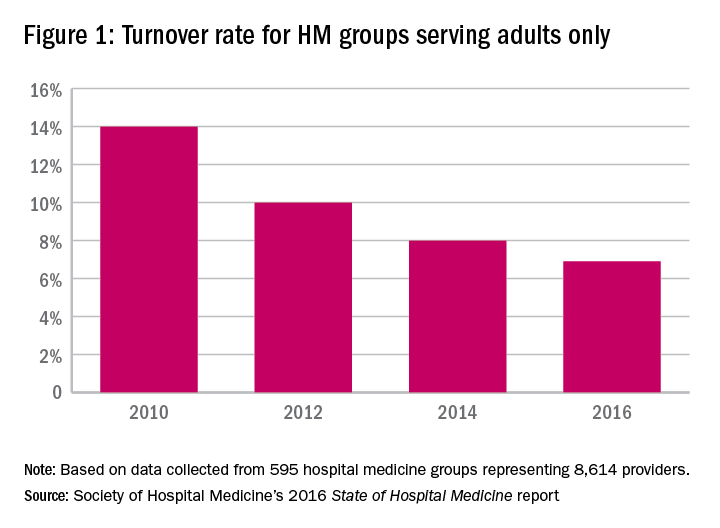
Turnover rate for hospitalist groups trending downward
According to the 2016 State of Hospital Medicine Report based on 2015 data, the median physician turnover rate for hospital medicine groups (HMGs) serving adults only is 6.9%, lower compared with results from prior surveys. Particularly, turnover in 2010 was more than double the current rate (see Figure 1). This steady decline over the years is intriguing, yet encouraging, since hospital medicine is well known for its high turnover compared to other specialties.
Similarly, results from State of Hospital Medicine surveys also reveal a consistent trend for groups with no turnover. As expected, lower turnover rate usually parallels with higher percentage of groups with no turnover. This year, 40.2% of hospitalist groups reported no physician turnover at all, continuing the upward trend from 2014 (38.1%) and 2012 (36%). It is speculating that these groups are not just simply fortunate, but rather work zealously to build a strong internal culture within the group and proactively create a shared vision, values, accountability, and career goals.
Sources in search of why providers leave a practice and advice on specific strategies to retain them are abundant. To secure retention, at a minimum, employers, leaders, or administrators should pay close attention to such basic factors as work schedules, workload, and compensation – and even consider using national and regional data from the State of Hospital Medicine Report for benchmarking to remain attractive and competitive in the market. Low or no turnover rate indicates workforce stability and program credibility, and allows cost saving as the overall estimated cost of turnover (losing a provider and hiring another one) ranges from $400,000 to $600,000 per provider.1
The turnover data further delineates differences based on academic status, Medicare Indirect Medical Education (IME) program status, and geographic region. For instance, the academic groups consistently report a higher turnover rate, compared with the nonacademic groups. The latter mirrors the overall decreasing trend of physician turnover. Non-teaching hospitals also score significantly higher on the number of groups with no turnover (42% as opposed to 24%-27% for teaching hospitals). Geographically, HMGs in the South and Midwest regions of the United States are the winners this year, with more than 50% of the groups reporting no turnover at all.
Specific information regarding turnover for nurse practitioners and physician assistants (NPs/PAs) can also be found in the report. This rate has been increasing slightly compared with the past, with a subsequent drop in the percentage of groups reporting no turnover. Yet, the overall percentage with no turnover for NPs/PAs remains impressively high at 62%.
The turnover rates for HMGs serving both adults and children, and groups serving children only, appear somewhat similar to those of groups serving adults only, though we cannot reliably analyze the data, elucidate significant differences, or detect any meaningful trends from these two groups because of insufficient numbers of responders.
The downward trend of hospitalist turnover found in SHM’s 2016 State of Hospital Medicine Report is reassuring, indicative of a higher retention rate and an extended stability for many programs. Although some hospitalists continue to shop around, most leaders and employers of HMGs work endlessly to strengthen their programs in hope to minimize turnover. The promising data likely reflect such effort. Hopefully, this trend will continue when the next State of Hospital Medicine report comes out.
Dr. Vuong is a hospitalist at HealthPartners Medical Group in St Paul, Minn., and an assistant professor of medicine at the University of Minnesota. He is a member of SHM’s Practice Analysis Committee.
Reference
1. Frenz, D (2016). The staggering costs of physician turnover. Today’s Hospitalist.