RIV poster contest a meeting highlight
Look back at the history of SHM’s annual Research, Innovations and Clinical Vignettes poster competition – better known as the RIV – and it may seem inevitable that it’s grown into one of the main highlights of the conference. The RIV has become so popular that the number of submissions has nearly tripled from 634 in 2010 to 1,712 this year.
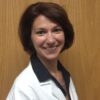
But inevitability has nothing to do with it, according to Margaret Fang, MD, MPH, FHM, and program chair for HM17’s scientific abstracts competition, which is RIV’s more formal sobriquet.
“Certainly, there is some natural evolution,” said Dr. Fang, a hospitalist, researcher, and anticoagulation clinic director at the University of California San Francisco. “But not all specialty societies embrace research or encourage its growth, so I would give a lot of credit to the Society of Hospital Medicine for being very deliberate in trying to strengthen its research program, highlight the research that hospitalists do, and make research a core pillar of what SHM stands for.”
The efforts have clearly worked, as RIV is a major driver for annual meeting attendance. The poster competition draws massive crowds that snake their way through the accepted posters.
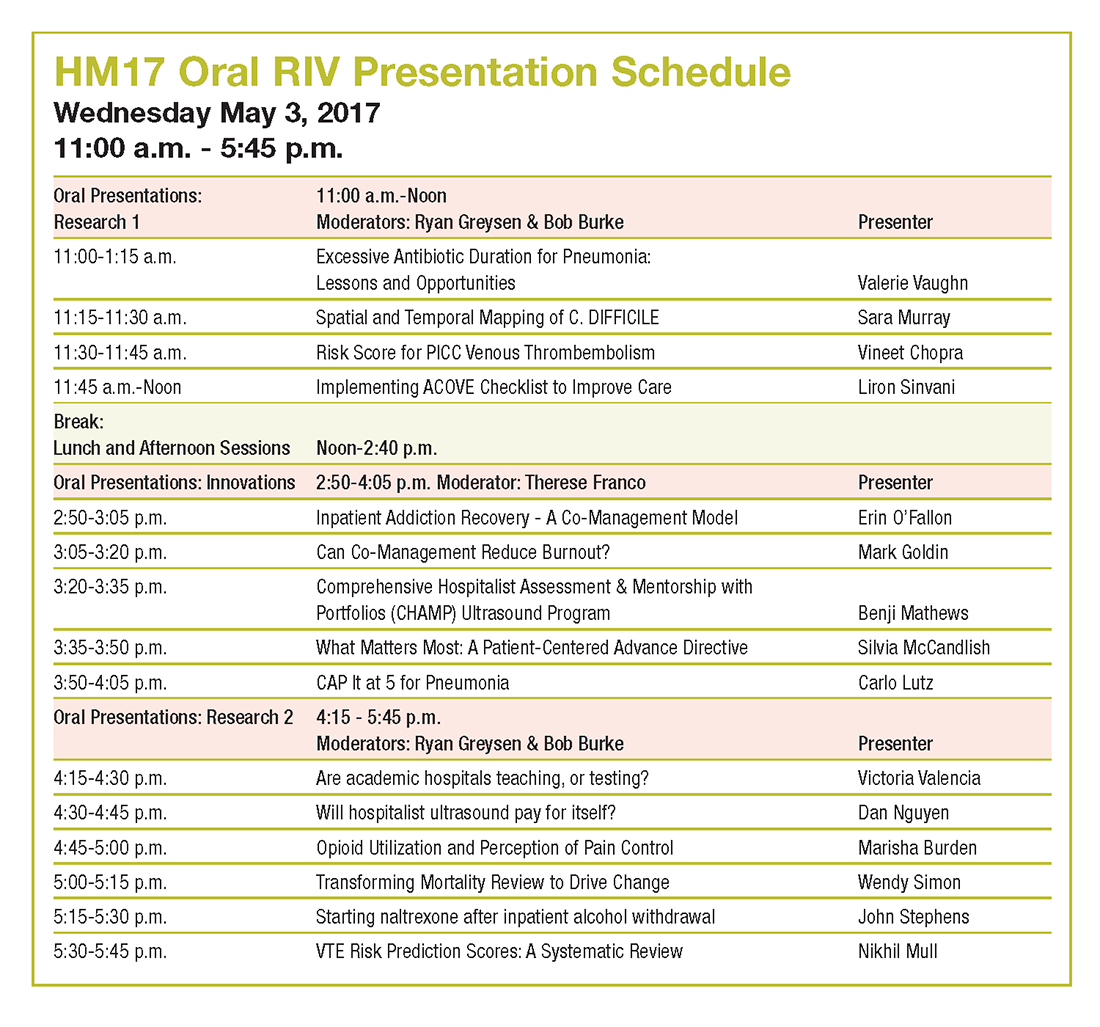
For those interested in a deeper dive, SHM chooses a dozen or so top abstracts for oral presentations that are, in Dr. Fang’s words, “the creme de la creme of all the research and innovations for the given year.”
The growth of the abstracts competition comes, of course, as the specialty itself has seen its ranks skyrocket. Hospitalists now number an estimated 52,000 nationally, and in addition to providing direct clinical care, have taken ownership of key health care drivers like patient safety, quality improvement, and systems change.
“We do what we do for the good of health care and, ultimately, for the good of our patients,” Dr. Fang said. “Sometimes that’s rounding and taking care of patients in a clinical fashion, and sometimes it’s contributing to the medical literature. It could have been really easy for a specialty to say, ‘Not our problem,’ or ‘No, we’re just rounding.’ ”
HM17 course director Lenny Feldman, MD, FACP, FAAP, SFHM, believes that the commitment of SHM’s founding generation to do research for the past decade has created a group of mentors that push younger hospitalists to do more of the same.
“If we didn’t have the research engine part of hospital medicine, if we didn’t have the folks who are getting into administration and other important leadership areas, we wouldn’t see the maturation of this specialty and we would, in many ways, be stuck at the point at which we started,” Dr. Feldman said. “The only way for us to move forward is to do the research, to be in position to make sure that hospital medicine continues to grow in a direction that is good for our patients, for us, and for the entire system.”
That perspective is what motivates hospitalists to make the RIV bigger each year, said Dr. Fang.
“Having your abstract accepted as a poster or an oral presentation showcases all the work that you’ve put into it,” Dr. Fang said. “There’s a huge amount of pride in showing what you’ve been able to achieve. The driving force is the desire to see what other people are doing, and network to share ideas. That’s the really wonderful part of the RIV competition.”