PIONEER-HF Extension: Don’t stall starting sacubitril/valsartan
NEW ORLEANS – Waiting a few months after a patient has been hospitalized for acute decompensated heart failure before launching a switch from enalapril to sacubitril/valsartan imposes a steep price in terms of extra major cardiovascular events, compared with starting the angiotensin-neprilysin inhibitor during the initial hospitalization, according to the open-label extension of the PIONEER-HF trial.
“We think these data have important clinical implications: While sacubitril/valsartan decreases NT-proBNP compared with enalapril regardless of when it is initiated, the early improvement in postdischarge outcomes supports the in-hospital initiation of sacubitril/valsartan in stabilized patients with acute decompensated heart failure,” Adam D. DeVore, MD, declared in presenting the PIONEER-HF Extension results at the annual meeting of the American College of Cardiology.
PIONEER-HF was a landmark, practice-changing, double-blind clinical trial in which 881 patients were randomized to initiation of sacubitril/valsartan (Entresto) or enalapril during hospitalization for acute decompensated heart failure. In the previously reported main outcome, 8 weeks after discharge the sacubitril/valsartan group had a 29% greater reduction in NT-proBNP (the N-terminal prohormone of brain natriuretic peptide) and a 42% lower rate of the composite clinical endpoint of cardiovascular death or heart failure rehospitalization than the enalapril group (N Engl J Med. 2019 Feb 7;380[6]:539-48).
The 4-week open-label extension of PIONEER-HF began at week 8, when participants initially randomized to enalapril during the double-blind phase were switched to sacubitril/valsartan, while those assigned to in-hospital initiation of the angiotensin-neprilysin inhibitor (ARNI) stayed the course.
At week 12, after 4 weeks of open-label treatment, patients on sacubitril/valsartan from the start experienced an additional 18.5% drop in NT-proBNP from their week-8 baseline of 1,218 pg/mL. Meanwhile, the NT-proBNP level in the switch group plunged by 35.8% from a week-8 baseline of 1,630 pg/mL. As a result, both groups ended up at the same much-improved biomarker level at week 12, observed Dr. DeVore, a cardiologist at Duke University in Durham, N.C.
Clinical event rates, however, were another story altogether. The clinical event gap between the two study arms documented at week 8 in the double-blind phase of the trial didn’t close significantly in the 4 weeks after the enalapril group crossed over to open-label sacubitril/valsartan. Indeed, the relative risk of the composite endpoint of cardiovascular death, heart failure rehospitalization, or left ventricular assist device implantation during the 4-week extension phase was 33% lower in the continuous sacubitril/valsartan group than in the switchers. The absolute risk reduction was 5.6%, with a favorable number needed to treat of 18.
This difference was driven mainly by less rehospitalization for heart failure. Few cardiovascular deaths or LVAD implantations occurred during the relatively brief 4-week extension phase of the trial.
“But this is an important thing as we think about what we’re trying to accomplish in heart failure: trying to find tools that improve rehospitalization rates after people leave the hospital is extremely important,” Dr. DeVore said. “We do know that the really vulnerable period for rehospitalization is early on, so my sus“`picion – though I can’t prove it – is that’s the important part. That’s when we need to have patients on the best therapy.”
He was asked how practical it is to initiate sacubitril/valsartan during hospitalization for acute decompensated heart failure in real-world clinical practice, given that it can be done only after patients achieve hemodynamic stability.
“I think the definition of hemodynamic stability we used in the trial was a fairly straightforward one, very clinical, and one we can translate to the bedside,” Dr. DeVore replied. “Patients had to have a systolic blood pressure of 100 mm Hg or greater for 6 hours, which is easily documented in the hospital, no changes in IV diuretics or IV vasodilators for 6 hours, and no IV inotropes for the last 24 hours. That’s how we defined hemodynamic stability. I think we should be able to find these patients.”
Average length of stay in the index hospitalization in PIONEER-HF was just over 5 days, but the study protocol actually resulted in longer-than-needed hospitalization because it required that patients had to receive three double-blind doses of their study medication before discharge. In routine practice, it’s unlikely that in-hospital initiation of sacubitril/valsartan will result in a length of stay greater than the national average of about 4.5 days, according the cardiologist.
Current ACC/American Heart Association/Heart Failure Society of American guidelines on management of heart failure include a Class Ia recommendation to switch patients from an ACE inhibitor or angiotensin inhibitor to sacubitril/valsartan (Circulation. 2017 Aug 8;136[6]:e137-61).
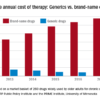
However, heart failure specialists are concerned by national data showing that sacubitril/valsartan remains widely underprescribed.
Dr. DeVore reported serving as a consultant to Novartis and receiving research grants from a half dozen pharmaceutical companies as well as the American Heart Association, National Heart, Lung, and Blood Institute, and the Patient-Centered Outcomes Research Institute .