 A 66-year-old man with a history of hypertension and stage 4 chronic kidney disease was admitted to the hospital for acute pulmonary embolism and started on a heparin drip. It is day two of his hospitalization, and your colleague has billed 99233 based on the 54 minutes they spent in the care of the patient today. You are called as cross-cover that evening to help with an issue involving multiple supratherapeutic activated partial thromboplastin time values. You make calls to phlebotomy, make changes to the orders, counsel the patient, speak with the nurse, and document what you have done, taking a total of 15 minutes in this care.
A 66-year-old man with a history of hypertension and stage 4 chronic kidney disease was admitted to the hospital for acute pulmonary embolism and started on a heparin drip. It is day two of his hospitalization, and your colleague has billed 99233 based on the 54 minutes they spent in the care of the patient today. You are called as cross-cover that evening to help with an issue involving multiple supratherapeutic activated partial thromboplastin time values. You make calls to phlebotomy, make changes to the orders, counsel the patient, speak with the nurse, and document what you have done, taking a total of 15 minutes in this care.
What billing does this qualify for?
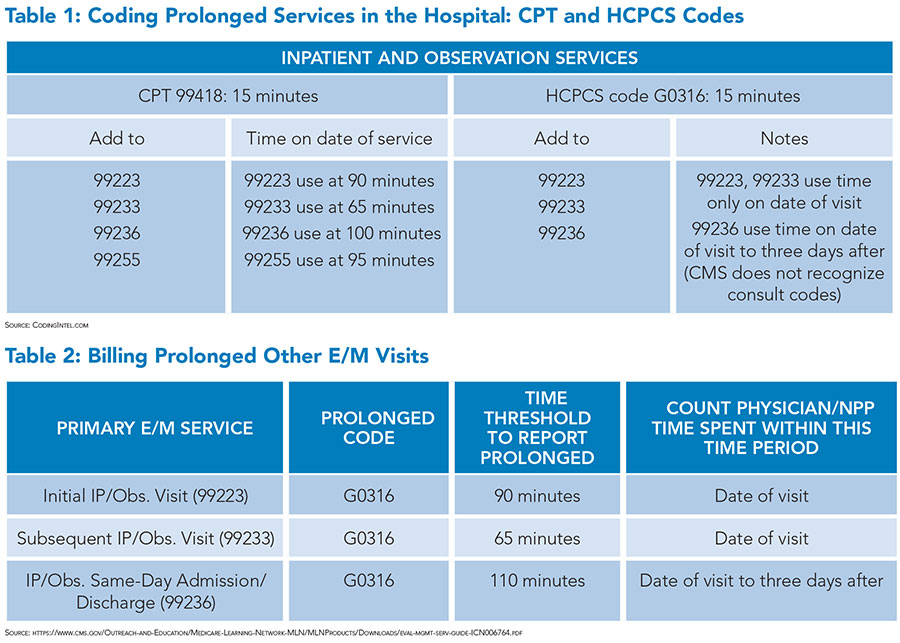
You can bill a prolonged services billing code 99418 (for non-Medicare patients) or G0316 (for Medicare patients). These codes can be used when the time for the care of the patient exceeds 15 minutes from the highest level of billing (by time). Thus, the minimum time needed for 99233 to be billed by time is 50 minutes, hence, 99418/G0316 can be used when the time exceeds 65 minutes for the calendar day in this case. You can add another such code if you exceed another 15 minutes for the calendar day (e.g., 80 minutes in this case). Each code grants you 0.61 work relative value units (wRVUs). (see Tables 1 and 2)
Dr. Mehta is the vice-chair of inpatient clinical affairs, medical director, and assistant professor of medicine in the clinical core faculty for program valuation and improvement at the University of Cincinnati Medical Center in Cincinnati, and the associate editor of The Hospitalist.
Can the prolonged care be billed and accepted /paid by a different hospitalist in the same day. Example . Patient admitted after midnight . Second hospitalist sees and modifies orders later in the same day . 2 providers bill one regular admission code time based , second provider only prolonged code based on the rules . How does the patient bill should be sent – all under one provider(first one) or both providers get credit ?
Yes, if the hospitalist is part of the same specialty and group, then yes, you can definitely add on time to the prior hospitalist’s billing charge. The challenge is usually when the first hospitalist bills by MDM criteria and does not list how much time they spent in the care of the patient. The bill will be sent under the providers’ group, unless the providers are not part of the same group.