The Power of Coaching

I am a mid-career academic hospitalist deeply interested in physician wellness and burnout. At SHM Converge 2025 in Las Vegas, I attended the wellness plenary by Dr. Sandeep Jauhar titled “Our Emotional Lives Are Written on Our Hearts: Health, Wellness, and Burnout in Clinical Practice Today” with great anticipation. While the session highlighted the alarming state of physician burnout, I found the conclusions unsatisfyingly vague. “So, what can we do, as healthcare professionals, to improve our lives and our health?” he asked the room.
A growing body of evidence offers an actionable response: get a coach.
Physician coaching is increasingly recognized as a transformative, strengths-based approach that empowers clinicians to develop clarity, resilience, and purpose in a demanding profession. Unlike advising, mentorship, or psychotherapy, coaching focuses on facilitating self-directed growth and insight. As it gains traction in academic and clinical settings, coaching has demonstrated measurable benefits in reducing burnout, enhancing professional fulfillment, and promoting adaptive leadership.1,2
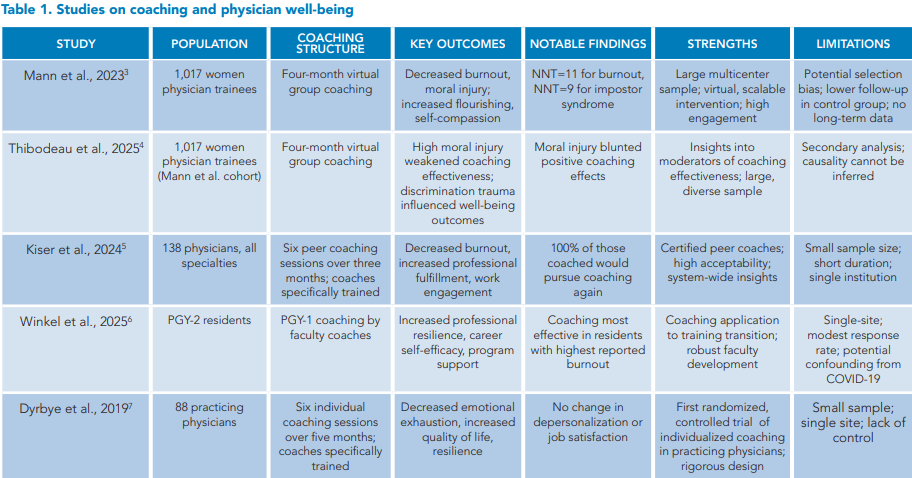
This article summarizes five published coaching interventions in medicine, highlighting various program designs, key outcomes, and lessons learned (see Table 1). These studies provide insight into how coaching can act as an effective lever for individual and organizational well-being.
The primary study by Mann et al. was a large, multicenter, randomized, clinical trial evaluating the impact of a four-month virtual group coaching program—Better Together Physician Coaching—on the well-being of 1,017 women physician trainees across 26 U.S. institutions.3 Participants randomized to the coaching group received live group video coaching, anonymous written coaching, and weekly self-directed modules. Compared to controls, coached participants experienced significant improvements in emotional exhaustion, depersonalization, impostor syndrome, moral injury, self-compassion, and overall flourishing. The number needed to treat was 11 to resolve one case of burnout and nine for impostor syndrome, highlighting the intervention’s clinical significance and scalability.
Building on this, Thibodeau et al. conducted a secondary analysis to explore how moral injury and discrimination trauma affected coaching outcomes within the same cohort.4 At baseline, higher moral injury was strongly associated with worse well-being across multiple measures. The analysis revealed that discrimination trauma moderated the relationship between moral injury and outcomes such as impostor syndrome and self-compassion, indicating that these two forms of distress interact and may compound each other. Post-intervention, while the coaching program was broadly effective, its positive effects were diminished in participants with high levels of moral injury, particularly in reducing impostor syndrome.
Together, these studies provide critical insight into the effectiveness and limitations of coaching interventions. While coaching can significantly enhance physician trainee well-being, its impact may be diminished in those facing unresolved systemic harms. The findings highlight the importance of pairing individual-level support with organizational and cultural changes that directly address discrimination and moral distress.
Kiser et al. conducted a randomized clinical trial to evaluate the impact of individualized peer coaching on physician burnout and well-being at the Massachusetts General Physicians Organization.5 A total of 138 physicians were randomized to receive either six individualized coaching sessions from certified physician peers over three months or standard institutional wellness resources. Among the intervention group, 52 completed at least one coaching session and were included in the modified intention-to-treat analysis.
Results showed statistically significant improvements among coached participants compared to controls. Notably, interpersonal disengagement decreased by 30.1%, overall burnout fell by 21.6%, professional fulfillment increased by 10.7%, and work engagement rose by 6.3%. Although changes in emotional exhaustion and depersonalization did not achieve significance, qualitative feedback and fidelity assessments indicated strong participant satisfaction and perceived value. Importantly, 100% of coached participants reported they would pursue coaching again.
The study highlights peer coaching as a viable, scalable, and cost-effective intervention. It not only benefited individual physicians but also showed potential for organizational impact, as themes emerging from coaching were shared with leadership and helped guide system-level initiatives. Although limitations included self-selection bias and a short follow-up period, the findings support integrating peer coaching into broader strategies to address physician burnout and foster workplace engagement.
The 2025 Winkel et al. study assessed the effects of a coaching program aimed at supporting medical students as they transitioned to residency at a single academic institution.6 The intervention, part of New York University’s Transition to Residency Advantage (TRA) program, involved faculty coaches meeting with residents throughout their intern year using a semi-structured, individualized approach. Researchers compared self-reported outcomes from this “coached” cohort to those of a prior “uncoached” cohort using validated scales for resilience, burnout, professional fulfillment, and program support.
Among 156 PGY-2 residents, survey responses (n=86) indicated that the coached group reported significantly higher levels of resilience, professional fulfillment, career self-efficacy, mentoring quality, and perceived institutional support. While both groups exhibited high engagement in self-directed learning habits, residents in the coached cohort demonstrated more positive attitudes toward goal setting. The positive effects of coaching were even more pronounced among residents who reported burnout, particularly in areas such as professional fulfillment and career support.
Although the study design cannot prove causality, the findings suggest that coaching may mitigate the negative effects of burnout and assist trainees in facing the professional and emotional challenges of early residency. Residents perceived coaching as having a moderately positive influence in various areas, including personal development and clinical decision making.
Dyrbye et al.’s randomized clinical trial, the first in individualized physician coaching, assessed the effectiveness of professional coaching in reducing burnout and improving well-being among physicians.7 A total of 88 physicians from Mayo Clinic were randomized to receive six sessions of one-on-one professional coaching over five months or no coaching. Coaching was provided by certified professionals and tailored to individual needs and goals.
Results indicated significant improvements in the coached group compared to the control group. Emotional exhaustion scores decreased (mean change: –5.2 points versus –1.5 points), and overall burnout was lower. Furthermore, coached physicians reported greater increases in quality of life and resilience. The coaching did not have a significant impact on depersonalization or job satisfaction, although trends were favorable.
This study demonstrates that individualized coaching is a promising intervention for reducing distress and promoting well-being among practicing physicians. By focusing on goal setting, self-reflection, and personal growth, coaching may serve as a valuable tool for addressing the widespread issue of physician burnout in clinical settings.
Summary
Recent research emphasizes the growing role of coaching as a strategy to enhance physician well-being throughout the training and practice continuum. These studies explore various coaching formats—from group-based to individualized, peer-delivered to professionally facilitated—and show that coaching positively impacts burnout, resilience, professional fulfillment, and career self-efficacy.
Several highlight that coaching may be particularly beneficial for those experiencing higher levels of distress, such as moral injury or early-career burnout, which is particularly relevant to hospital medicine, given published wellness data.8 Emerging themes in these studies include the importance of psychological safety, the ability to reveal systems-based issues through physician coaching, and the feasibility of scaling interventions through virtual or peer-led models. Collectively, this body of work reflects a shift to viewing physician coaching as a practical, evidence-based component of physician support and professional development rather than a luxury.
 Dr. Sankey is an associate professor of medicine at Yale School of Medicine and the director of Yale’s academic program in hospital medicine. He is the co-chief of Yale’s Hospital Medicine Firm, program director of the adult hospital medicine fellowship program, faculty director of the resident elective in hospital medicine, and a certified Wellcoach and physician coach for Yale medical students, all in New Haven, Conn.
Dr. Sankey is an associate professor of medicine at Yale School of Medicine and the director of Yale’s academic program in hospital medicine. He is the co-chief of Yale’s Hospital Medicine Firm, program director of the adult hospital medicine fellowship program, faculty director of the resident elective in hospital medicine, and a certified Wellcoach and physician coach for Yale medical students, all in New Haven, Conn.
References
1. Stephany AM, et al. Professional coaching in medicine and health care. Clin Sports Med. 2023;42(2):195-208. doi: 10.1016/j.csm.2022.11.001.
2. Schulte EE. enhancing leadership and faculty development: the benefits of coaching for physicians and physician leaders. J Pediatr. 2024;268:113827. doi: 10.1016/j. jpeds.2023.113827.
3. Mann A, et al. Online well-being group coaching program for women physician trainees: a randomized clinical trial. JAMA Netw Open. 2023;6(10):e2335541. doi: 10.1001/jamanetworkopen.2023.35541.
4. Thibodeau P, et al. The moderating effects of moral injury and discrimination trauma on women physician trainees’ well-being. J Gen Intern Med. 2025;40(11):2679-2686. doi: 10.1007/s11606- 025-09434-5.
5. Kiser SB, et al. Physician coaching by professionally trained peers for burnout and well-being: a randomized clinical trial. JAMA Netw Open. 2024;7(4):e245645. doi: 10.1001/jamanetworkopen.2024.5645.
6. Winkel AF, et al. Evaluating the impact of coaching through the transition to residency. J Gen Intern Med. 2025;40(1):10-16. doi: 10.1007/s11606-024-08865-w.
7. Dyrbye LN, et al. Effect of a professional coaching intervention on the well-being and distress of physicians: a pilot randomized clinical trial. JAMA Intern Med. 2019;179(10):1406-1414. doi: 10.1001/jamainternmed.2019.2425.
8. 2023 State of Hospital Medicine Report. Society of Hospital Medicine website. https://education.hospitalmedicine.org/Listing/2023-State-of-Hospital-Medicine-Report-Electronic-Print-Version-9342. Published 2023. Accessed December 27, 2025.